Table of Contents
Context: World Tuberculosis Day is observed on 24th March annually. Indian Researchers have developed an indigenous, cost-effective and real-time LAMP (rt-LAMP) assay for early diagnosis of Tuberculosis.
| About rt-LAMP Assay |
|
About Tuberculosis (TB)
- Tuberculosis is a bacterial infection spread through inhaling tiny droplets from the coughs or sneezes of an infected person.
- Caused by: a bacterium called Mycobacterium tuberculosis, belonging to the Mycobacteriaceae family.
- Transmission: Person to person through the air.
- When people with lung TB cough, sneeze or spit, they propel the TB germs into the air.
- Affects: In humans, TB most commonly affects the lungs (pulmonary TB), but it can also affect other organs (extra-pulmonary TB).
- Curable?: Treatable and curable disease.
| Drug-Resistant TB |
|
| Facts on Tuberculosis (TB) in India |
|
India’s Efforts in Eliminating TB
Strengthening Diagnosis and Treatment
Expansion of molecular testing for rapid detection of TB and drug resistance.
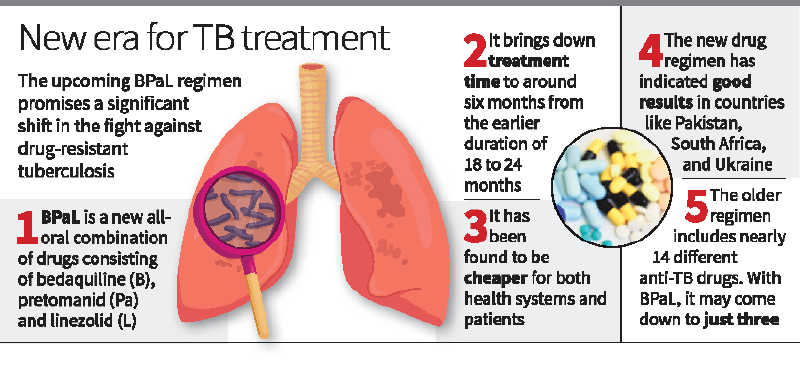
- Introduction of the shorter, all-oral BPaLM regimen (Bedaquiline, Pretomanid, Linezolid, and Moxifloxacin) for drug-resistant TB.
- Launch of the 100 Days’ campaign for intensive case finding.
- Establishment of a diagnostics network to optimise sample collection and transportation.
Nutritional and Financial Support
- Ni-kshay Poshan Yojana (NPY) entitlement doubled to ₹1,000 per month for nutritional support.
- AB-PMJAY offers full insurance coverage for TB care in both public and private sectors.
- Efforts to reduce out-of-pocket expenditure (OOPE) through social protection schemes.
Decentralisation of TB Care
TB services integrated within Ayushman Bharat under:
- Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) – for secondary and tertiary care.
- Ayushman Arogya Mandirs (AAMs) – for primary care, including sputum collection and referral services.
Training of community health officers at AAMs to handle TB cases at the grassroots level.
Community Engagement and Support
- Involvement of TB Champions (TB survivors) for patient counselling and support.
- Community-based interventions like Tamil Nadu Kasanoi Erappila Thittam (TN-KET) for early referral and reduced TB mortality.
Equity and Targeted Interventions
Adoption of a gender-responsive approach to TB care under NTEP.
- Targeted outreach to vulnerable groups like tribal communities, migrants, and homeless populations.
- Early work to address TB and disability through improved understanding of health vulnerabilities.
Awareness and Public Engagement
- Strengthened public awareness campaigns to address TB stigma and misinformation.
- Focus on drug-resistant TB and antimicrobial resistance (AMR).
100-day Intensified TB Mukt Bharat Abhiyaan (Launched on December 7, 2024)
- Targeted Screening: Portable X-ray machines targeted high-risk groups like diabetics, smokers, alcohol consumers, HIV patients, the elderly, and TB patient contacts.
- AI-Powered Diagnosis: AI-based X-rays flagged suspected cases instantly, and confirmed them through Nucleic Acid Amplification Tests (NAAT).
- Widespread Reach: The campaign screened 12.97 crore vulnerable individuals, identifying 7.19 lakh TB cases, including 2.85 lakh asymptomatic cases.
Also Read: Elimination Of Tuberculosis (TB)
Challenges That Still Persist
- High Burden and Slow Decline in Incidence: TB incidence declined from 237 per 100,000 (2015) to 195 per 100,000 (2023) – but this pace is inadequate to meet the target of TB elimination by 2025.
- Delayed Diagnosis and Treatment: Over 50% of TB patients still seek care in the private sector with uneven standards of care.
- Diagnostic delays, improper treatment, and mismanagement in the private sector contribute to drug resistance.
- Out-of-Pocket Expenditure (OOPE): Despite AB-PMJAY and NPY, indirect costs like wage loss, transport, and caregiver support remain high.
- Financial burden increases the risk of treatment non-compliance and relapse.
- Poor Health System Integration: Lack of integrated screening for other diseases (e.g., COPD, diabetes) in TB patients.
- Weak referral linkages between private and public health systems.
- Stigma and Social Barriers: TB patients continue to face social stigma, especially women and vulnerable groups.
- Stigma discourages people from seeking care and completing treatment.
- Limited Outreach to Marginalised Groups: Tribal, migrant, and homeless populations remain underserved due to geographical and socio-economic barriers.
- Health-seeking behavior among marginalised groups is influenced by cultural and logistical challenges.
What Needs to be Done
Strengthen Early Detection and Diagnosis
Scale up rapid molecular testing at primary health centres (PHCs).
- Expand AI-based chest X-rays and upfront molecular testing.
- Introduce incentives for early reporting and diagnosis in the private sector.
Ensure Complete Financial Protection
Expand AB-PMJAY coverage to include all indirect costs like wage loss, transport, and caregiver support.
- Pilot livelihood programmes for TB survivors.
- Increase NPY entitlement for those from economically weaker backgrounds.
Improve Private Sector Engagement
Introduce a standardised TB treatment protocol for the private sector.
- Establish a mandatory referral system for TB cases detected in private facilities.
- Offer incentives to private healthcare providers for compliance with NTEP guidelines.
Strengthen Decentralisation and Integration
Improve diagnostic, treatment, and referral systems at Ayushman Arogya Mandirs.
- Train community health workers to handle co-morbidities like COPD, diabetes, and depression.
- Ensure uniform standards of care across rural and urban centres.
Address Stigma and Awareness Gaps
Launch a targeted TB awareness campaign using the successful COVID-19 communication model.
- Promote community-led engagement to reduce stigma and misinformation.
- Encourage TB Champions to lead awareness drives at the grassroots level.
Targeted Support for Vulnerable Groups
Develop tailored strategies for tribal and migrant communities.
- Provide mobile TB care units in remote and underserved areas.
- Ensure gender-sensitive and culturally appropriate TB care delivery.

 AI and its Regulation in India, Limitati...
AI and its Regulation in India, Limitati...
 Silicon Photonics Enables Low-power AI A...
Silicon Photonics Enables Low-power AI A...
 Genome India Project (GIP), Aim and Sign...
Genome India Project (GIP), Aim and Sign...