Table of Contents
Context: The West Bengal Chief Minister has proposed a Shorter Medical Course for medical practitioners who would serve in primary health centers (PHCs) in rural areas.
More on the News
- This proposal seeks to tackle the persistent scarcity of doctors in rural areas, where a substantial proportion (approximately 65%) of the Indian population resides.
- Other states, like Chhattisgarh, have already implemented similar initiatives, such as a three-year community health program that trains Rural Medical Assistants (RMAs) to cater to the healthcare needs of villages.
Understanding the proposed Shorter Medical Course
- The proposed shorter medical course for rural areas in India is a three-year diploma course specifically designed for medical practitioners who would serve in primary health centers (PHCs) located in rural regions.
- It differs from the regular MBBS (Bachelor of Medicine, Bachelor of Surgery) course in terms of duration, curriculum focus, and level of specialization.
Objectives
- The objective of the shorter medical course is to equip healthcare providers with the necessary skills to deliver primary-level care in rural areas.
- It aims to address the shortage of doctors in these regions by providing a targeted and expedited training program.
- While the regular MBBS course covers a comprehensive range of medical subjects and prepares doctors for various medical scenarios, the shorter medical course emphasizes first-level care and basic medical practices required in rural settings.
- It aims to increase the availability of medical professionals in rural areas, ensuring a more rapid response to healthcare needs and emergencies.
Benefits of the proposed shorter medical course include:
- Increased availability of medical professionals in rural areas, alleviating the doctor shortage.
- Prompt and efficient healthcare response to the specific needs of rural communities.
- Cost-effectiveness, as the shorter course can be a viable solution for resource-constrained regions.
- Enhanced primary healthcare services in rural communities, leading to improved overall health outcomes.
Drawbacks
- Limited specialization in complex medical fields, as the focus is primarily on providing basic care.
- Insufficient exposure to the diverse range of healthcare conditions prevalent in rural areas.
- Concerns about potential dilution of medical education standards compared to the comprehensive MBBS course.
- The potential for discrimination, as there may be concerns about less qualified healthcare providers being assigned to rural populations while urban areas receive more highly qualified practitioners.
- The proposed shorter medical course does not directly address underlying structural issues contributing to the shortage of doctors in rural areas.
Rural Health Statistics report for 2021-22
According to the Rural Health Statistics report for 2021-22, there is an acute shortage of specialist doctors in rural areas of India, particularly at Community Health Centers (CHCs).
Key highlights:
- Shortage of Specialists: The report reveals that nearly 80% of the required specialist doctors are unavailable at CHCs. The specific specialties experiencing a shortfall include surgeons (83.2%), obstetricians and gynaecologists (74.2%), physicians (79.1%), and paediatricians (81.6%).
- Increase in Specialist Doctors: While the number of specialist doctors at CHCs has increased by 25% over the years, from 3,550 in 2005 to 4,485 in 2022, this growth has not been sufficient to meet the rising demand for specialists in rural areas.
- Lack of Female Health Workers: In addition to the shortage of specialist doctors, there is also a dearth of female health workers and auxiliary nursing midwives in primary health centers (PHCs) and sub-centers, with up to 14.4% of these positions remaining vacant.
- Challenges: The status of doctors in rural India, as per the report, indicates significant challenges in addressing the shortage of doctors in rural areas. These challenges include inadequate infrastructure and resources, limited access to specialized care, an aversion to rural practice among doctors, unequal distribution of medical colleges, difficulties in retaining rural doctors, socioeconomic factors, and educational disparities.
Healthcare Infrastructure in India
- Health infrastructure is an important indicator for understanding the healthcare delivery provisions and welfare mechanisms in a country.
- Infrastructure has been described as the basic support for the delivery of public health activities. Public health infrastructure has been referred to as ‘the nerve center of the public health system’.
- Article 47 of the Constitution of India mandates improvement in public health, thus the government is required to take all measures for this purpose.
- The National Health Mission followed by National Health Policy 2017 lays a major thrust on addressing the infrastructural needs and gaps. National Health Policy further recommends strengthening of the regulatory role of MOHFW in the regulation of clinical establishments and professional & technical education.

Types of Public Healthcare Infrastructure Services
Indian public health system has a three-tier system of healthcare service –
- Primary Health Services: Primary health care is the basic level of health care which includes programs focused on the elevation of health, the initial diagnosis of disease or ill health, and deterrence of illness. It involves the key healthcare structure which delivers the first level of interaction between the healthcare providers and the population. E.g., Sub Centres (SCs) and Primary Health Centres (PHCs).
- Secondary health care: It is at an intermediate level of health care which comprises diagnosis and treatment, accomplished in a hospital with particular tools and laboratory facilities. The secondary health care structure exists at the Community Health Centres (CHCs), urban hospitals and district hospitals.
- Tertiary Health Services: It is a particular and extremely practical level of health care which comprises diagnosis and cure of disease and disability. Tertiary Health care services refer to the third level of the health system which is mostly focused and advice-giving care is being provided frequently on recommendation from primary and secondary medicinal care. Tertiary care is available mostly in Medical College Hospitals super-speciality hospitals and rehabilitation centres. These are found mainly in state capitals and other Bigger cities.
Why Primary health care is important?
- Primary health interventions help detect diseases early, well before complications set in.
- It reduces the need for expensive secondary and tertiary healthcare.
- Of the total current expenditure on health classified by healthcare functions, preventive care accounts for 6.7 per cent, while spending on curing people account for 51% of the total expenditure on health.
- Developed nations such as the UK, Australia, Canada, Netherlands and Sweden spend a large share of their federal healthcare budgets on primary care.
- India has been spending huge amount in cure of non-communicable diseases, which can only be won through a primary health system that ensures that chronic diseases are not only detected early, but also that preventive action is taken to ensure improved lifestyles.
- Unavailability of PHC from government leads to heavy burden of out of pocket expenses on consultations and drugs.
Problems of PHC in India
- Limited services: Although Primary Health Care system exists in India but its scope is limited to pregnancy care, limited childcare and certain services related to national health programmes.
- Training and manpower problems: PHCs are suffering from poor management skills, lack of appropriate training and supportive supervision for health workers.
- Conversion in Health and Wellness centres: Government announced conversion of 150,000 sub centres into HWCs in 2017 budget and also in National Health policy 2017, only few thousand such centres have been sanctioned.
- Urban neglect: Primary Health care for growing urban population has not been conceptualized. It’s focus is still limited to the rural population of India.
- Funding: Funding for overall health care is very low, leaving insufficient amount that requires to be spend on Primary Health Care.
- Staff shortage: PHCs are also suffering from inadequate skilled and trained manpower. There is a shortfall of about 9,000 doctors in about 25,000 PHCs in the country.
- Poor facilities: Primary level facilities need complete building reconstruction, as they operate out of rented apartments and thatched accommodations, and lack basic facilities such as toilets, drinking water and electricity.
- Overburdened PHCs: India has a large network of primary health centres (PHCs), each supposed to serve a population of 25,000. But in states such as Madhya Pradesh, Bihar and Jharkhand, however, a PHC covers as many as 45,000, 49,000 and 76,000 people.
Government Measures
- The National Health Policy (NHP) 2017 advocated allocating resources of up to two thirds of total health budget to Primary Health care.
- Last year, an outlay of ₹1,200 crore was proposed to transform 1.5 lakh sub-health centres into health and wellness centres(HWC) by 2022, which would provide a wider range of primary care services than existing sub and primary health centres (PHC).
- Each HWC is to be operated by a well-trained, mid-level health provider (nurse practitioner or community health officer) who will be supported by a team of front line health workers to provide an expanded package of services.
Best National and International Practices
- Cuba has one of the most effective primary healthcare systems in the world, the system provides community-based polyclinic, each polyclinic serves a catchment area hosting between 30,000 and 60,000 people.
- Polyclinic facility is further extended by neighbourhood-based family doctor-and-nurse offices closer to the communities, one such office for 1,000-2,000 people. Prevention is the cornerstone of these services, complemented by community analysis and treatment.
- In a cross-country analysis of governance systems and health outcomes, countries with higher fiscal decentralisation (Citizens participation) were found to have consistently lower infant mortality rates that those with more centralised forms.
- In West Bengal and Kerala in India – states in which primary healthcare is co-managed by panchayats – health outcomes are better than in most other states at similar levels of economic development.


 World Population Day 2025, Themes, Histo...
World Population Day 2025, Themes, Histo...
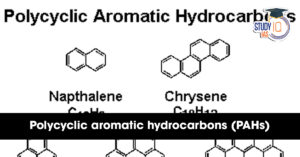 What are Polycyclic Aromatic Hydrocarbon...
What are Polycyclic Aromatic Hydrocarbon...
 Marlin Fish: Species, Features, Appearan...
Marlin Fish: Species, Features, Appearan...