Table of Contents
Gene Therapy
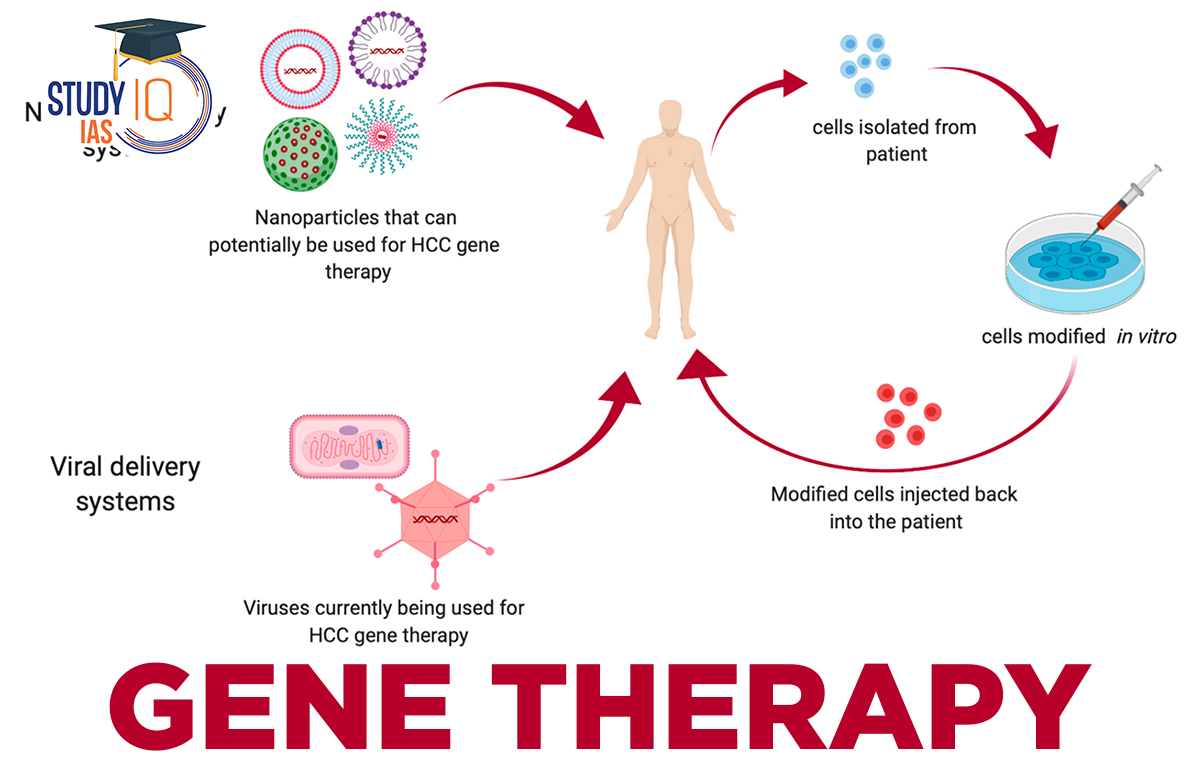
- Gene therapy is a medical method that treats or prevents disease by correcting the underlying genetic problem.
- Doctors use techniques to alter a person’s genetic makeup instead of using drugs or surgery.
T-cell Acute Lymphoblastic Leukemia
- It is a type of blood cancer in which the T-cells turn against the body and destroy healthy cells that normally help with immunity.
- It is a rapid and progressive disease and is usually treated by chemotherapy and radiation therapy.
- T-cells are a class of white blood cells that are equipped to hunt and neutralize threats to the body.
More on the News
- The patient had tried several of the standard treatments including chemotherapy and radiation with limited success.
- The patient then enrolled in a new experimental trial and became the first to receive experimental gene therapy that relied on a new technique called ‘base editing.’
What is Base Editing?
- A person’s genetic code is made up of combination of four bases— Adenine (A), Guanine (G), cytosine (C) and thymine (T).
- Sequences of these bases give instructions to genes to produce the wide array of proteins necessary for the body’s functions.
- Sometimes because of a mis-arrangement in the sequence of bases, wrong instructions are passed, making cells malfunction. Cells can also turn cancerous.
- Base editing technique allows genes to be altered and errors fixed by making changes at the bases. CRISPR-cas 9 system is the most popular method of gene editing.
- In this case, researchers improvised the technique to be able to directly change certain bases: thus, a C can be changed into a G and T into an A.
- Applications: Base editing is more effective at treating blood disorders which are caused by so-called single point mutations. These mutations can cause terminal disease.
Using Base Editing to Treat T-cell Leukemia
- The main objective behind gene therapy in the case of T-cell leukemia was to fix immune system in a way that it stops making cancerous T-cells.
- In the first step, healthy T-cells were extracted from a donor and put through a series of edits.
- The first edit changed T-cells targeting mechanism so it would stop attacking patient’s body.
- The second edit removed a chemical marking, called CD7, which is present on all T-cells.
- The third edit prevented the cells being killed by a chemotherapy drug.
- The T-cells were programmed to kill all cells — cancerous or protective — with CD7 marker.
- After a few days, the patient was given a second donor transplant to regrow immune system containing healthy T-cells.
- Effectiveness:
- After three months of the treatment, investigation does not suggest any signs of the disease resurfacing.
- However, it still cannot be established if treatment has reliably and entirely fixed the immune system.

 Sir Shankaran Nair and Story of the Jall...
Sir Shankaran Nair and Story of the Jall...
 What are Atmospheric Rivers?
What are Atmospheric Rivers?
 Cheetah Project Steering Committee Key R...
Cheetah Project Steering Committee Key R...