Table of Contents
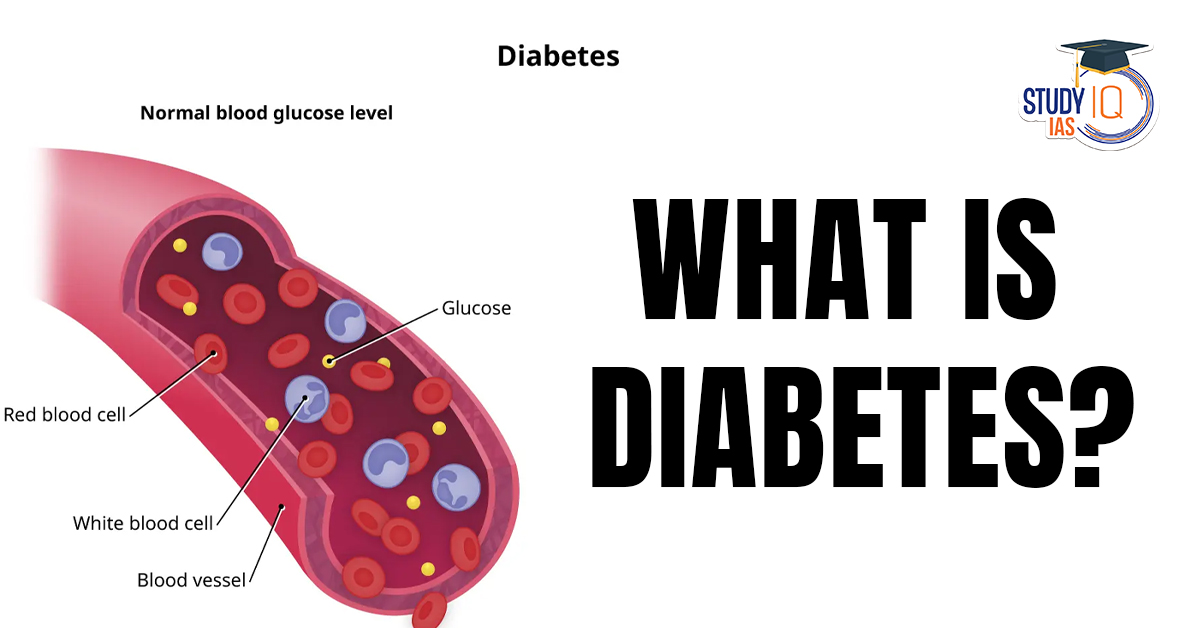
In a groundbreaking move, the International Diabetes Federation (IDF) has recognized Type 5 Diabetes as a distinct form of diabetes that is driven by malnutrition, rather than excess sugar. This new classification highlights a growing global health concern and provides much-needed attention to a diabetes variant primarily found in low- and middle-income countries. Unlike the more commonly known Type 1 and Type 2 diabetes, Type 5 Diabetes arises from poor nutrition and developmental issues during childhood, leading to underdeveloped pancreatic function.
What is Type 5 Diabetes?
Type 5 Diabetes is a form of diabetes that is primarily caused by malnutrition and chronic undernutrition. It generally affects lean, malnourished teenagers and young adults, especially in regions with limited access to proper nutrition, including many low- and middle-income countries.
Key Characteristics of Type 5 Diabetes:
-
It is not caused by excess sugar intake or insulin resistance.
-
It is a result of poor pancreatic development during pregnancy due to nutritional deficiencies.
-
It leads to insulin deficiency due to underdeveloped pancreatic beta cells, which are responsible for insulin production.
Origin and Early Recognition:
-
Type 5 Diabetes was first identified in Jamaica in 1955 and was initially referred to as J-type diabetes. Researchers observed that the condition disproportionately affected young adults in areas where undernutrition was prevalent.
-
In recent years, it has gained more recognition as a malnutrition-related form of diabetes, primarily seen in countries with poor access to nutrition and high rates of childhood undernutrition.
How Does Type 5 Diabetes Develop?
Unlike Type 1 Diabetes, which is an autoimmune disorder that attacks the insulin-producing cells of the pancreas, and Type 2 Diabetes, which results from insulin resistance, Type 5 Diabetes develops differently:
-
Prenatal Underdevelopment: The roots of Type 5 Diabetes begin in the womb. Chronic undernutrition during pregnancy affects the fetus’s pancreas development, leading to a deficiency of pancreatic beta cells that are crucial for producing insulin after birth.
-
Insulin Deficiency: As a result, pancreatic beta cells in individuals with Type 5 diabetes produce very little insulin. This is not because the body is resistant to insulin or attacks its own cells, but simply because the pancreas did not develop fully due to inadequate nutrition.
-
Impact on Metabolism: Without enough insulin, the body cannot properly regulate blood sugar levels, leading to hyperglycemia (high blood sugar). This condition affects young people, typically manifesting during teenage years or early adulthood.
Risk Factors and Affected Population
Type 5 Diabetes primarily affects young people in regions where malnutrition is prevalent. The risk is higher among:
-
Children born to malnourished mothers.
-
Young adults and teenagers from low-income countries or regions are experiencing food insecurity.
-
Communities affected by chronic hunger and poor maternal health.
Affected Regions:
-
Many parts of Africa, South Asia, and Latin America experience a higher prevalence of Type 5 Diabetes due to chronic undernutrition and food scarcity.
Symptoms and Diagnosis of Type 5 Diabetes
The symptoms of Type 5 Diabetes can resemble those of other forms of diabetes, but the underlying causes are distinct. Common symptoms include:
-
Excessive thirst and frequent urination.
-
Fatigue and weakness.
-
Unexplained weight loss despite normal or excessive food intake.
-
Blurred vision.
-
Slow healing of wounds.
Diagnosis typically involves:
-
Blood tests to measure blood glucose levels.
-
Evaluation of medical history and nutritional status.
-
Exclusion of Type 1 and Type 2 diabetes based on the patient’s unique health profile.
Treatment and Management
While Type 5 Diabetes involves insulin deficiency, its management differs from Type 1 and Type 2 diabetes due to the root cause being malnutrition. Treatment often involves:
-
Dietary interventions to address underlying malnutrition.
-
Insulin therapy to regulate blood sugar levels, as needed.
-
Nutritional support for proper growth and pancreatic development.
-
Monitoring of blood glucose levels to ensure proper control.
Long-Term Outlook:
Type 5 Diabetes requires long-term management, but with the right nutrition and care, individuals can live healthy lives. Early intervention, particularly during the developmental years, is crucial to prevent further complications.
Conclusion
The recognition of Type 5 Diabetes by the International Diabetes Federation (IDF) marks a significant step forward in understanding diabetes in a global context. As the world grapples with the challenges of malnutrition and food insecurity, Type 5 Diabetes brings attention to the need for better maternal health and nutritional policies, particularly in developing nations. Awareness and early detection are key to managing this form of diabetes and preventing its lifelong consequences for vulnerable populations.

 World Immunization Week (24 to 30 April)...
World Immunization Week (24 to 30 April)...
 National Panchayati Raj Day (24th April)...
National Panchayati Raj Day (24th April)...
 Digital Bharat Nidhi Boost to Rural Tele...
Digital Bharat Nidhi Boost to Rural Tele...