Table of Contents
Context: The UNICEF (United Nations International Children’s Emergency Fund), WHO (World Health Organization) and the World Bank have jointly published the Joint Malnutrition Estimates (JME) 2023 report.
What are Joint Malnutrition Estimates (JME)?
- The UNICEF-WHO-World Bank JME Working Group was established in 2011 to harmonize child malnutrition estimates across countries.
- The inter-agency team releases annual child malnutrition estimates for the indicators stunting, wasting, overweight and underweight.
- The first edition of the JME was released in 2012. The key findings in the 2023 edition include global and regional trends for all mentioned indicators as well as country-level modeled estimates.
What are the key findings of the report for India?
| Child Stunting |
|
| Child Wasting |
|
| Child Overweight |
|
What is Child Malnutrition?
- Child malnutrition may be defined as a pathological state resulting from inadequate nutrition, including:
- Undernutrition (protein-energy malnutrition) due to insufficient intake of energy and other nutrients. There are several sub-forms of undernutrition: wasting, stunting, and underweight.
- Overnutrition (overweight and obesity) due to excessive consumption of energy and other nutrients.
- Hidden hunger i.e., Deficiencies of essential vitamins and minerals – often referred to as micronutrients.

Major Factors Contributing to Child Malnutrition in India
- Insufficient Access to Healthy Food: Limited availability and access to nutritious food contribute to both undernutrition and overnutrition, increasing the risks of low birthweight, childhood stunting, and overweight or obesity.
- Feeding Habits and Lack of Nutritional Awareness: Inadequate knowledge about the nutritional value of food, misconceptions, inappropriate child rearing and feeding practices contribute to undernutrition within families.
- Poverty: Poverty restricts the purchasing power of individuals, making it difficult for them to afford an adequate quantity and quality of food for their families. This creates a vicious cycle of poverty, undernutrition, reduced work capacity, low income, and continued poverty.
- Infections: Diseases like malaria, measles, and recurring bouts of diarrhea can precipitate acute malnutrition and exacerbate existing nutritional deficiencies.
- Maternal Anemia: Undernourished mothers often give birth to undernourished babies, leading to a worsening rate of malnutrition. Difficulties in accessing proper nutrition benefits contribute to this issue.
- Migration: Families migrating to cities in search of better livelihoods often find themselves excluded from government schemes that are primarily delivered at the local level.
- Socio-cultural Factors:
- Inequitable Food Distribution within Families: In many poor households, women and young children, especially girls, receive less food compared to economically active male members.
- Large Families: Frequent pregnancies negatively impact the nutritional status of mothers, resulting in low birthweight babies. Additionally, large families often face limited per capita availability of food.
- Poor Quality of Housing, Sanitation, and Water Supply: Inadequate living conditions contribute to ill health, infections, and subsequent malnutrition.
Impacts of Child Malnutrition
- Impaired Physical Growth: Malnutrition, especially undernutrition, can result in stunted growth and delayed physical development.
- Cognitive and Intellectual Impairment: Malnourished children often suffer from cognitive and intellectual impairments, including difficulties with learning, memory, attention, and problem-solving. These effects can hinder educational attainment and limit future opportunities.
- Increased Risk of Chronic Diseases: Malnourished children are at a higher risk of developing chronic diseases later in life, such as diabetes, cardiovascular diseases, and obesity.
- Economic impact: Undernutrition reduces economic advancement due to losses in productivity, poorer cognition, and poorer educational outcomes. Iron deficiency reduces children’s ability to learn.
- India loses up to 4% of its gross domestic product and 8% of its productivity due to child malnutrition.
Initiatives taken by Government
- Integrated Child Development Scheme and the Anganwadi system — to provide supplementary nutrition and ration to pregnant and lactating women, run mid-day meal scheme in schools and maternity benefit programme.
- The National Food Security Act 2013 assures food and nutrition security to the vulnerable and that access to food is a legal right.
- National Nutrition Strategy (NITI Aayog) aims to reduce all forms of malnutrition by 2030, with a focus on the most vulnerable and critical age groups.
- POSHAN Abhiyaan to achieve improvement in nutritional status of Adolescent Girls, Pregnant Women and Lactating Mothers in a time bound manner.
- Mission POSHAN 2.0 seeks to address the challenges of malnutrition in children, adolescent girls, pregnant women, and lactating mothers.
Way Forward
- Nutrition Education and Awareness: Raising awareness about the importance of balanced diets, optimal infant and young child feeding practices, and the nutritional value of different foods.
- Better Food Systems: Improving children’s nutrition requires food systems to deliver nutritious, safe, affordable, and sustainable diets for all children.
- Diversifying food production: by moving away from mono cropping of major cereals to a system that integrates a variety of food items including small millets, pulses, fruits, and vegetables.
- Fortification of complementary foods and staple foods: with micronutrients can be a cost-effective intervention to combat hidden hunger in children.
- Strengthen Maternal and Child Health Services: Particularly during pregnancy, childbirth, and the early years of a child’s life. This includes providing adequate antenatal care, promoting breastfeeding, ensuring proper nutrition during pregnancy, and delivering essential micronutrients and supplements to mothers and children.


 World Population Day 2025, Themes, Histo...
World Population Day 2025, Themes, Histo...
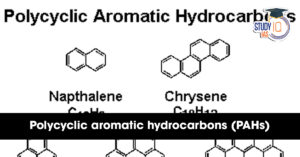 What are Polycyclic Aromatic Hydrocarbon...
What are Polycyclic Aromatic Hydrocarbon...
 Marlin Fish: Species, Features, Appearan...
Marlin Fish: Species, Features, Appearan...