Table of Contents
Inheritance and Sex Determination
Introduction
It has been observed that reproductive processes give rise to new individuals who share similarities yet possess subtle differences. In this chapter, we will delve into the mechanism responsible for the creation and inheritance of variations. Additionally, we will consider the intriguing implications of accumulating variations over time, which will be studied within the context of evolution.
Genetics
Genetics is the scientific field that studies how traits and characteristics are passed from one generation to another. It encompasses the study of genes, which are segments of DNA (deoxyribonucleic acid) that contain the instructions for building and maintaining an organism. These genes determine various aspects of an organism’s physical traits, such as eye color, height, and susceptibility to certain diseases.
Inheritance
Inheritance refers to the process by which genetic information, encoded in genes, is passed from parents to offspring. It involves the transmission of traits, characteristics, and genetic variations from one generation to the next. These traits can include physical characteristics like eye colour, hair texture, and height, as well as susceptibility to certain diseases or conditions.
In sexual reproduction, the genetic material (DNA) from two parents is combined through the fusion of gametes (sperm and egg cells), resulting in offspring that inherit a combination of genetic traits from both parents. This leads to genetic diversity and the potential for new variations within a population.
Heredity
Heredity, also known as genetics, involves the transfer of genetic traits from parents to their offspring. It is the pattern of transfer of traits which is at the core of heredity. Also, variation lies at the heart of heredity, as it encompasses the diversity and range of genetic traits that can be inherited.
|
Difference between Inheritance and Heredity |
|
| Inheritance | Heredity |
| Describes the process of transferring genetic traits from parents to offspring. | Refers to the transmission and expression of genetic characteristics from one generation to another. |
| Focuses on the pathway of genetic traits and how they are passed down through generations. | Encompasses the overall concept of genetic transmission, including inheritance as a specific aspect. |
| Deals with the specific patterns of genetic traits being transmitted from parents to offspring. | Encompasses both the patterns and variations of genetic traits being passed down through generations. |
| Can involve both Mendelian inheritance (single gene traits) and complex inheritance patterns (polygenic traits). | Encompasses all types of genetic inheritance, including Mendelian, non-Mendelian, and epigenetic factors. |
| Emphasizes the passing down of specific genetic traits or characteristics. | Considers the broader scope of genetic information and its impact on the overall characteristics of individuals. |
| Plays a role in understanding genetic disorders, traits, and their patterns of expression in offspring. | Provides insights into the genetic basis of inherited diseases, phenotypic variations, and the evolution of populations. |
Mendel’s Laws of Inheritance
Gregor Mendel, often referred to as the father of modern genetics, formulated three fundamental laws of inheritance based on his experiments with pea plants. These laws, known as Mendel’s Laws of Inheritance, laid the foundation for understanding the patterns and mechanisms of genetic inheritance. The three laws are:
- Law of Dominance
- Law of Segregation
- Law of Independent Assortment
Mendel’s laws provided a framework for understanding the mechanisms of genetic inheritance and helped explain the patterns of traits observed in his experiments. These laws laid the groundwork for the development of modern genetics, including the concepts of genes, alleles, dominance, recessiveness, and the principles of inheritance that still hold true today.
Significance of Inheritance
- Genetic Diversity: Inheritance contributes to the genetic diversity within a species. It allows for the combination and recombination of genetic material during sexual reproduction, leading to the generation of unique genetic variations in each offspring. This genetic diversity is essential for the survival and adaptation of populations to changing environments.
- Evolutionary Processes: Inheritance plays a central role in the process of evolution. Genetic variations inherited from parents can provide advantages or disadvantages in terms of survival and reproduction. Through natural selection, individuals with beneficial traits are more likely to pass on their genes to the next generation, leading to the gradual accumulation of favorable traits over time.
- Inherited Traits and Characteristics: Inheritance determines the transmission of specific traits and characteristics from parents to their offspring. These traits can include physical attributes such as eye color, height, and hair texture, as well as predispositions to certain diseases or disorders. Understanding inherited traits is crucial for studying genetic disorders, identifying risk factors, and developing targeted treatments.
- Medical Implications: Inheritance plays a vital role in medical genetics. Inherited genetic mutations or variations can contribute to the development of genetic diseases or increase susceptibility to certain conditions. Studying inheritance patterns helps in diagnosing genetic disorders, understanding disease inheritance risks, and developing strategies for prevention and treatment.
- Agricultural and Plant Breeding: Inheritance is of great significance in agriculture and plant breeding. By selectively breeding plants and animals with desirable traits, such as high crop yield or disease resistance, inherited traits can be manipulated to enhance agricultural productivity and improve food security.
- Forensic Applications: Inheritance forms the basis of genetic fingerprinting and DNA profiling in forensic science. Inherited genetic markers can be used to establish biological relationships, identify individuals, and provide evidence in criminal investigations.
Sex determination
The question of how the sex of a newborn individual is determined as different species employ diverse strategies in this regard. Some rely solely on environmental cues. For instance, in certain animals, the temperature at which fertilized eggs are kept dictates the development of male or female individuals within the eggs.
In contrast, some animals, like snails, possess the ability to change their sex, indicating that sex is not determined by genetics alone. However, in the case of human beings, our sex is predominantly determined by our genetic makeup. Put simply, the genes inherited from our parents play a significant role in determining whether we will be male or female.
Sex Determination in Humans
It is determined by the presence or absence of specific sex chromosomes inherited from the parents. Chromosomes are thread-like structures found within the nucleus of cells that carry genetic information in the form of DNA (deoxyribonucleic acid). Chromosomes play a crucial role in cell division and inheritance.
The sex determination process in humans:
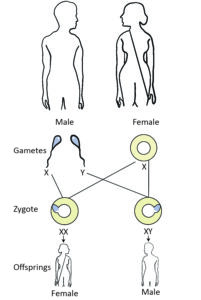
- Sex Chromosomes: Humans have 23 pairs of chromosomes, including two sex chromosomes, known as X and Y chromosomes. Females typically have two X chromosomes (XX), while males have one X and one Y chromosome (XY).
- Inheritance of Sex Chromosomes: During reproduction, each parent contributes one sex chromosome to their offspring. The mother always passes on an X chromosome, while the father can pass on either an X or a Y chromosome.
- Male Sex Determination: If the father contributes an X chromosome, the resulting combination (XX) leads to the development of a female offspring. However, if the father contributes a Y chromosome, the combination (XY) leads to the development of male offspring. The presence of the Y chromosome triggers the development of male reproductive structures.
- Sex Chromosome Anomalies: While XX and XY are the typical sex chromosome combinations, there can be variations and anomalies. For example, some individuals may have additional copies of sex chromosomes (e.g., XXY, XYY) or atypical combinations (e.g., XO, where only one X chromosome is present in females). These variations can lead to differences in sexual development and may be associated with certain conditions or syndromes.
- Genetic Basis: The genes located on the sex chromosomes play a role in the development of sexual characteristics and reproductive organs. The SRY gene, located on the Y chromosome, is considered the “sex-determining region” and triggers the development of male characteristics.
It’s important to note that while sex determination in humans is primarily based on genetic factors, there are other biological and environmental factors that can influence sexual development, such as hormonal influences during fetal development. The interplay between genetic and environmental factors can contribute to the complexity of sexual development and variations in sexual characteristics among individuals.
Sex determination techniques
Sex determination techniques for fetuses are used during prenatal testing to determine the sex of the unborn baby. Some commonly employed techniques are:
- Ultrasound: Ultrasound imaging is a non-invasive technique that uses high-frequency sound waves to create images of the developing fetus.
- During an ultrasound examination, the genital area of the fetus can be visualized, allowing the technician or doctor to determine the presence of male or female genitalia.
- This method is typically used after the 16th week of pregnancy and is considered safe and reliable for sex determination.
- Non-Invasive Prenatal Testing (NIPT): NIPT is a blood test that analyzes fetal DNA present in the mother’s bloodstream.
- This test can detect and analyze specific genetic markers, including those associated with the sex chromosomes.
- By examining the presence of X and Y chromosomes, NIPT can determine the biological sex of the fetus with high accuracy.
- NIPT is usually performed after the 9th week of pregnancy and carries a low risk of complications.
- Chorionic Villus Sampling (CVS) and Amniocentesis: These invasive procedures involve the collection of fetal cells for genetic testing.
- CVS is performed between the 10th and 12th week of pregnancy, while amniocentesis is typically performed between the 15th and 20th week.
- These tests are primarily used for detecting chromosomal abnormalities and genetic disorders but can also provide information about the fetus’s sex.
| Illegal Sex Determination in India – PCPNDT Act,1994 |
| The Pre-Conception and Pre-Natal Diagnostic Techniques (PCPNDT) Act is an Indian legislation enacted in 1994, with subsequent amendments in 2003, 2002, and 2014. The act aims to regulate and prevent the misuse of prenatal diagnostic techniques for sex determination, thereby addressing the issue of female feticide and promoting gender equality.
The key provisions of the PCPNDT Act include: Prohibition of Sex Determination: The act prohibits the use of any technique or procedure for determining the sex of the fetus, except for medical reasons prescribed by a qualified medical professional. Registration of Genetic Counseling Centers, Genetic Laboratories, and Genetic Clinics: The act mandates the registration and regulation of facilities that conduct prenatal diagnostic procedures. These centers, laboratories, and clinics must comply with the prescribed standards and maintain proper records. Prohibition of Advertisements: The act prohibits advertisements, whether in print or electronic media, promoting prenatal diagnostic techniques for determining the sex of the fetus. This provision aims to curb the promotion of sex-selective practices. Prohibition of Sale of Ultrasound Machines: The act restricts the sale, distribution, or use of ultrasound machines for any purpose other than medical diagnosis. This provision is aimed at preventing the unauthorized use of ultrasound machines for sex determination. Penal Provisions and Penalties: The act imposes strict penalties on those found violating its provisions. It includes imprisonment, fines, cancellation of registration, and closure of facilities involved in illegal practices related to sex determination. The PCPNDT Act is significant in addressing the issue of female feticide, which has led to imbalanced sex ratios in India. By regulating the use of prenatal diagnostic techniques and prohibiting sex determination, the act seeks to protect the lives of female fetuses and promote gender equality. It emphasizes the importance of prenatal diagnostics for medical purposes while discouraging its misuse for illegal sex determination. |
Chromosomal Theory of Inheritance
The chromosomal theory of inheritance, also known as the Sutton-Boveri theory, is a fundamental concept in genetics that explains how genetic traits are passed from one generation to the next through chromosomes. This theory was proposed independently by Walter Sutton and Theodor Boveri in the early 20th century. The chromosomal theory of inheritance states the following key points:
- Genes are located on chromosomes: The theory suggests that genes, the units of heredity, are located on chromosomes. Genes are specific segments of DNA that carry instructions for the development and functioning of organisms.
- Chromosomes carry genetic information: Chromosomes are the vehicles that carry and transmit genetic information from one generation to the next. During cell division, chromosomes replicate and distribute their genetic material to daughter cells.
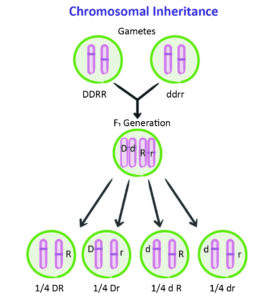
- Homologous chromosomes and alleles: In sexually reproducing organisms, individuals inherit two copies of each chromosome, one from each parent. These chromosome pairs, called homologous chromosomes, carry the same genes at corresponding locations (loci), although they may have different versions of those genes called alleles. For example, there may be one allele for eye color inherited from the mother and a different allele for eye color inherited from the father.
- Mendelian principles apply to chromosomes: The principles of inheritance described by Gregor Mendel, known as Mendelian genetics, can be explained by the behavior of chromosomes. Mendel’s laws, such as the law of segregation and the law of independent assortment, can be understood in terms of the separation and recombination of chromosomes during meiosis, the process of cell division that produces gametes (sperm and eggs).
- Chromosome segregation and recombination: The chromosomal theory explains how chromosomes segregate and recombine during meiosis. During meiosis, homologous chromosomes pair up, exchange genetic material through a process called crossing over, and then separate into different cells. This segregation and recombination of chromosomes during meiosis result in the formation of genetically diverse gametes.
Limitations of the chromosomal theory of inheritance
- Non-Mendelian Inheritance: The theory cannot fully explain inheritance patterns involving interactions between multiple genes or non-chromosomal factors.
- Presence of Non-Coding DNA: The theory focuses on genes but doesn’t fully account for the functional significance and complexity of non-coding DNA.
- Epigenetic Modifications: The theory does not fully consider the influence of epigenetic modifications on gene expression and inheritance patterns.
- Chromosome Variations: The theory assumes typical diploid organisms, but variations in chromosome structure and number can affect inheritance in unique ways.
- Non-Chromosomal Inheritance: The theory does not encompass inheritance through non-chromosomal elements like mitochondrial DNA or cytoplasmic factors.
Significance of Chromosomal Theory of Inheritance
- The chromosomal theory of inheritance provides a framework for understanding how genetic traits are inherited and passed on from parents to offspring.
- It helped unify the fields of genetics and cytology by establishing the connection between the behavior of chromosomes and the patterns of inheritance observed by Mendel.
- This theory laid the foundation for further discoveries in genetics and paved the way for our current understanding of the role of chromosomes in heredity.
Genetic disorders
Genetic disorders, also known as genetic diseases or genetic conditions, are disorders that result from abnormalities or mutations in an individual’s genes or chromosomes. These abnormalities can affect the structure, function, or regulation of genes, leading to a wide range of health problems and medical conditions.
There are thousands of different genetic disorders, and they can affect various aspects of an individual’s health, including physical characteristics, metabolism, organ function, and susceptibility to certain diseases. Examples of genetic disorders include cystic fibrosis, Down syndrome, sickle cell anemia, Huntington’s disease, and hemophilia.
Causes of genetic disorders
- Inherited Genetic Mutations: Genetic disorders can result from inherited genetic mutations passed down from parents. Examples include cystic fibrosis, sickle cell anemia, and Huntington’s disease.
- Spontaneous Genetic Mutations: Genetic disorders can arise from spontaneous genetic mutations that occur randomly during the formation of sperm or egg cells or early fetal development. Examples include Down syndrome and achondroplasia.
- Chromosomal Abnormalities: Genetic disorders can be caused by changes in the number or structure of chromosomes. Examples include Turner syndrome and Klinefelter syndrome.
- Environmental Factors: Certain environmental factors, such as exposure to chemicals, toxins, or infections during pregnancy, can contribute to the development or severity of genetic disorders. An example is fetal alcohol syndrome.
- Multifactorial Inheritance: Some genetic disorders result from a combination of genetic susceptibility and environmental triggers. Examples include heart disease, diabetes, and cleft lip and palate.
Some important genetic disorders are:
A) Chromosomal disorders
Down syndrome
Down syndrome, also known as trisomy 21, is a genetic disorder caused by the presence of an extra copy of chromosome 21. It is one of the most common chromosomal disorders, occurring in approximately 1 in 800 births.
The main characteristic features of individuals with Down syndrome include distinctive facial appearance, such as almond-shaped eyes, a flattened facial profile, and a small nose and mouth. They may also have low muscle tone, developmental delays, and intellectual disabilities of varying degrees.
Turner syndrome
Turner syndrome, also known as 45,X or monosomy X, is a genetic disorder that affects females. It occurs when one of the sex chromosomes, typically the X chromosome, is missing or partially missing. Instead of the usual two X chromosomes (XX), individuals with Turner syndrome have only one normal X chromosome (X0).
Klinefelter syndrome
Klinefelter syndrome is a genetic disorder that affects males and is characterized by the presence of an extra X chromosome. Most males have one X and one Y chromosome (46,XY), but individuals with Klinefelter syndrome have an additional X chromosome (47,XXY).
B) Monogenic disorders
Monogenic disorders, also known as monogenic or single-gene disorders, are genetic disorders caused by mutations or abnormalities in a single gene. Unlike complex genetic disorders, which involve the interaction of multiple genes and environmental factors, monogenic disorders are primarily caused by alterations in a specific gene. Few examples of monogenic diseases:
Cystic Fibrosis
Cystic fibrosis is a genetic disorder caused by mutations in the CFTR (Cystic Fibrosis Transmembrane Conductance Regulator) gene. It primarily affects the lungs, pancreas, and other organs, resulting in thick, sticky mucus production and impaired organ function.
Huntington’s Disease
Huntington’s disease is an autosomal dominant disorder caused by mutations in the HTT (Huntingtin) gene. It leads to the progressive degeneration of nerve cells in the brain, resulting in movement disorders, cognitive decline, and psychiatric symptoms.
Duchenne Muscular Dystrophy
Duchenne muscular dystrophy is an X-linked recessive disorder caused by mutations in the DMD (Dystrophin) gene. It primarily affects males and leads to the progressive degeneration of muscle fibers, resulting in muscle weakness and wasting.
Sickle Cell Anemia
Sickle cell anemia is a recessive genetic disorder caused by mutations in the HBB (Beta-Globin) gene. It affects the structure and function of red blood cells, leading to the characteristic sickle shape, reduced oxygen-carrying capacity, and various complications.
Hemophilia
Hemophilia is an X-linked recessive disorder caused by mutations in genes such as F8 (Factor VIII) or F9 (Factor IX). It affects the blood’s ability to clot properly, leading to prolonged bleeding and increased susceptibility to internal and external bleeding.
Marfan Syndrome:
Marfan syndrome is an autosomal dominant disorder caused by mutations in the FBN1 (Fibrillin-1) gene. It affects connective tissue, leading to abnormalities in the skeletal system, cardiovascular system, eyes, and other organs.
C) Mitochondrial disorders
Mitochondrial disorders are a group of genetic disorders that affect the mitochondria, which are the energy-producing structures within cells. These disorders can result from mutations in either nuclear DNA or mitochondrial DNA (mtDNA). Since mitochondria have their own DNA separate from the nucleus, and is inherited only from mother, these disorders can be inherited from the mother specifically. Examples of Mitochondrial Disorders:
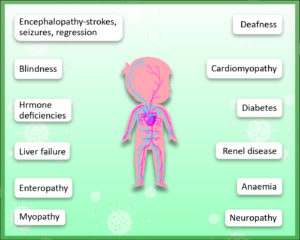
Leigh syndrome
This is a severe neurodegenerative disorder that typically begins in infancy or early childhood. It causes progressive neurological deterioration, muscle weakness, and movement abnormalities.
MELAS
Mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes (MELAS) is characterized by recurrent stroke-like episodes, seizures, muscle weakness, and lactic acid buildup in the blood.
Mitochondrial myopathy
This refers to a group of disorders that primarily affect the muscles, leading to muscle weakness, exercise intolerance, and fatigue.
Leber’s hereditary optic neuropathy (LHON)
LHON specifically affects the optic nerves, causing sudden vision loss, typically in young adults.
D) Polygenic disorders
Polygenic disorders, also known as complex disorders, are conditions that result from the combined effects of multiple genes and environmental factors. Unlike monogenic disorders, which are caused by mutations in a single gene, polygenic disorders involve the interaction of multiple genetic variants, each contributing a small effect, along with environmental factors. Many common diseases and conditions are considered polygenic disorders. Examples include:
Diabetes mellitus
Both type 1 and type 2 diabetes involve the interaction of multiple genes and environmental factors in the development of the disease.
Cardiovascular diseases
Conditions such as coronary artery disease, hypertension, and stroke have a polygenic basis, with multiple genes influencing the risk.
Obesity
Obesity is influenced by the interplay of genetic factors and environmental factors such as diet and physical activity.
Asthma
Asthma is a complex disorder with genetic and environmental components contributing to its development and severity.
Treatment of Genetic Disorders- Gene Therapy
Gene therapy is a promising field of medical research that aims to treat genetic disorders by introducing genetic material into a person’s cells to correct or replace the faulty genes responsible for the disorder. The ultimate goal of gene therapy is to restore normal gene function, thereby treating the underlying cause of the genetic disorder.
There are several technologies used in gene therapy to deliver therapeutic genes into the cells of the body. Some of the key techniques are:
- Viral Vectors: Viral vectors are the most commonly used vehicles for delivering therapeutic genes in gene therapy. Viruses, such as retroviruses, lentiviruses, adenoviruses, and adeno-associated viruses (AAVs), are modified to carry the therapeutic gene and deliver it to the target cells. These viruses have been engineered to be safe and non-pathogenic, and their ability to infect cells and integrate their genetic material into the host genome is exploited for gene delivery.
- Non-viral Vectors: Non-viral vectors are another approach in gene therapy that involves the direct introduction of therapeutic genes into cells without the use of viruses. These vectors can be in the form of plasmid DNA, naked DNA, liposomes, nanoparticles, or other synthetic carriers. Non-viral vectors are typically less immunogenic and have a larger cargo capacity compared to viral vectors, but they are generally less efficient in gene delivery.
- CRISPR-Cas9 Technology: CRISPR-Cas9 is a revolutionary gene-editing technology that has opened new possibilities for gene therapy. It enables precise editing of genes by cutting the DNA at specific locations and introducing desired genetic changes. CRISPR-Cas9 can be used to correct disease-causing mutations, insert therapeutic genes, or disrupt malfunctioning genes. This technology has shown promise in treating various genetic disorders, although it is still being refined and optimized for clinical applications.
- Ex Vivo vs. In Vivo Gene Therapy: Gene therapy can be performed ex vivo or in vivo, depending on the approach and the type of cells being targeted. Ex vivo gene therapy involves removing cells from the patient, modifying them with the therapeutic gene in the laboratory, and then reintroducing the genetically modified cells back into the patient’s body. In vivo gene therapy, on the other hand, involves directly delivering the therapeutic genes to the target tissues or cells within the patient’s body.
The development and application of gene therapy face several challenges, including efficient and specific gene delivery, immune responses, off-target effects, and long-term safety and efficacy. However, significant progress has been made, and gene therapy has shown success in treating certain genetic disorders, such as severe combined immunodeficiency (SCID), inherited retinal diseases, and certain types of leukemia.
Gene therapy holds immense potential for the treatment of various genetic disorders, but further research, clinical trials, and technological advancements are still needed to improve its safety, efficiency, and accessibility. Regulatory agencies closely monitor gene therapy research and ensure that it follows strict ethical guidelines and safety protocols.
Out of the above mentioned, we will discuss the CRISPR-Cas 9 technology in detail.
CRISPR-Cas9
CRISPR-Cas9 is a revolutionary gene-editing technology that allows precise modifications to be made to the DNA of living organisms. It stands for Clustered Regularly Interspaced Short Palindromic Repeats and CRISPR-associated protein 9. The CRISPR-Cas9 system is derived from the immune system of bacteria, where it acts as a defense mechanism against viral infections.
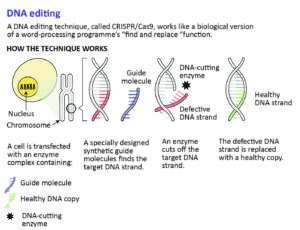
Features of CRISPR-Cas9 technology
- How it works: CRISPR-Cas9 uses a guide RNA molecule that is designed to match a specific target sequence in the DNA. The Cas9 enzyme acts as molecular scissors and cuts the DNA at the targeted site. Once the DNA is cut, the cell’s natural repair mechanisms can be harnessed to introduce desired genetic changes.
- Gene Editing Capabilities: CRISPR-Cas9 allows for several types of genetic modifications. The most common are:
- Gene Knockout: The DNA is cut at a specific location, disrupting the target gene’s function.
- Gene Insertion: New genetic material can be inserted at the targeted site.
- Gene Correction: Specific disease-causing mutations can be repaired or corrected.
- Versatility and Precision: CRISPR-Cas9 is highly versatile and can be used in various organisms, including animals, plants, and microorganisms. Its precision in targeting specific DNA sequences makes it a powerful tool for genetic research and potential therapeutic applications.
Applications
- Basic Research: CRISPR-Cas9 is widely used in laboratories for studying gene function, disease mechanisms, and developmental processes.
- Therapeutic Potential: CRISPR-Cas9 has the potential to treat genetic disorders by correcting disease-causing mutations. It offers possibilities for developing personalized medicine and targeted therapies.
- Agriculture: CRISPR-Cas9 can be used to enhance crop traits, improve agricultural productivity, and develop disease-resistant plants.
- Biotechnology: It enables the production of genetically modified organisms with specific traits, such as improved yields or enhanced tolerance to environmental conditions.
The use of CRISPR-Cas9 in humans raises important ethical considerations, including concerns about unintended off-target effects, germline editing (altering DNA that can be inherited by future generations), and the potential for misuse or inappropriate use.
CRISPR-Cas9 technology has revolutionized genetic research and has the potential to significantly impact medicine, agriculture, and biotechnology. Ongoing research is focused on refining its efficiency, specificity, and safety, as well as addressing ethical and regulatory concerns.
Mitochondrial Replacement therapy
Mitochondrial replacement therapy (MRT), also known as mitochondrial donation or three-parent IVF, is a reproductive technique aimed at preventing the transmission of certain mitochondrial disorders from mother to child. Mitochondrial disorders are genetic conditions caused by mutations in the mitochondrial DNA (mtDNA), which can lead to various health problems.
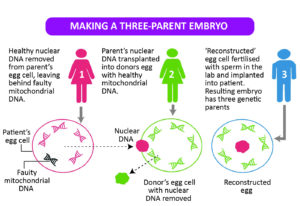
Features of mitochondrial replacement therapy:
- Purpose: MRT is primarily used to help families with a high risk of passing on mitochondrial disorders to have healthy children. By replacing the faulty mitochondria in the mother’s egg with healthy mitochondria from a donor, the resulting embryo will have most of its genetic information from the parents but with healthy mitochondria.
- Techniques: There are different techniques used in MRT, including pronuclear transfer and maternal spindle transfer. The pronuclear transfer involves transferring the nucleus of a fertilized egg from the affected mother into a donor egg that has had its nucleus removed but retains its healthy mitochondria. Maternal spindle transfer involves transferring the nuclear DNA from the mother’s egg to a donor egg with healthy mitochondria before fertilization.
- Mitochondrial DNA: Mitochondria are the energy-producing structures within cells and have their own small amount of DNA, separate from the nuclear DNA. Mitochondrial disorders result from mutations in the mtDNA, which can affect the proper functioning of mitochondria and lead to a range of health issues, including muscle weakness, organ dysfunction, and neurological problems.
- Success and Limitations: MRT has shown promising results in preventing the transmission of mitochondrial disorders, with healthy children born through these techniques. However, MRT is not a guarantee of a disease-free outcome, as it cannot address nuclear DNA mutations or other genetic factors that may contribute to the disorder. Furthermore, long-term safety data and the potential effects on offspring are still being studied.
Pronuclear transfer
Pronuclear Transfer offers a means to prevent the transmission of mitochondrial diseases to offspring since mitochondrial DNA is inherited exclusively from the mother. In this technique, the mother’s egg is initially fertilized with sperm, resulting in the formation of a zygote.
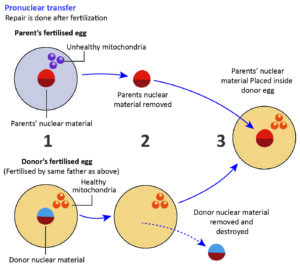
The pronuclei (under-developed nucleus) from the egg and sperm are subsequently extracted from the zygote and transferred into a donor egg that has already been fertilized and had its nucleus removed. Finally, the zygote derived from the donor egg, containing the combined genetic material, is implanted into the mother’s uterus.
Sexual and Asexual Reproduction
Reproduction and its Significance
Reproduction is the biological process by which new individuals of a species are produced, ensuring the continuation and survival of that species over time. It is a fundamental process in the life cycle of organisms and is significant for the following purposes:
- Species Continuity: Reproduction allows for the perpetuation of a species, ensuring that it remains viable and does not become extinct. Through reproduction, new individuals are produced to replace those that have died, maintaining a stable population.
- Genetic Diversity: Reproduction promotes genetic diversity within a species. Sexual reproduction, in particular, involves the combination of genetic material from two parents, resulting in offspring with unique genetic characteristics. This diversity is essential for the adaptation and survival of a species in changing environments.
- Evolutionary Adaptation: Reproduction is intimately linked to the process of evolution. Genetic variation resulting from reproduction allows for the occurrence of favorable traits that enhance an organism’s survival and reproductive success. Over time, these advantageous traits become more prevalent in a population, leading to evolutionary adaptations.
- Growth and Development: Reproduction is crucial for the growth and development of individual organisms. Through reproduction, new individuals are generated, starting from single cells and progressing through various stages of development, ultimately becoming mature and capable of reproducing themselves.
- Ecosystem Functioning: Reproduction plays a vital role in maintaining the balance and functioning of ecosystems. Different organisms, including plants, animals, and microorganisms, reproduce to ensure ecological diversity, energy flow, and the stability of food chains and ecological interactions.
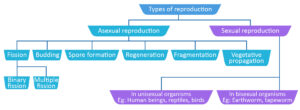
Types of Reproduction
The two major types of reproduction are sexual reproduction and asexual reproduction.
Sexual Reproduction
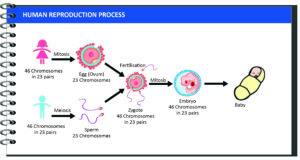
Sexual reproduction involves the fusion of gametes, which are specialized reproductive cells, from two parent organisms. This process requires the involvement of both males and females. It typically involves the following steps:
- Gamete Production: Males produce sperm cells, while females produce egg cells (ova).
- Fertilization: The sperm and egg unite during sexual intercourse or through external fertilization, resulting in the formation of a zygote with a complete set of genetic information.
- Genetic Variation: Sexual reproduction introduces genetic variation as the offspring inherit a combination of genetic material from both parents. This genetic diversity contributes to the adaptability and survival of the species in changing environments.
- Offspring Development: The zygote develops into an embryo, which further develops into a fetus and eventually a new individual is born.
Asexual Reproduction
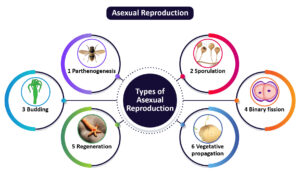
Asexual reproduction involves the production of offspring without the involvement of gametes or the fusion of genetic material. It is typically carried out by a single-parent organism and does not require a mate. Asexual reproduction methods include:
- Binary Fission: The parent organism divides into two equal parts, each becoming a separate individual (e.g., bacteria).
- Budding: An offspring develops as an outgrowth or bud from the parent organism, eventually detaching and becoming independent (e.g., yeast, hydra).
- Fragmentation: The parent organism breaks into fragments, with each fragment capable of developing into a new individual (e.g., starfish, planarians).
- Vegetative Reproduction: New individuals develop from vegetative structures like rhizomes, runners, or plant bulbs (e.g., strawberries, potatoes).
- Parthenogenesis: Development of offspring from unfertilized eggs (e.g., certain insects, reptiles, and plants).
While sexual reproduction provides genetic diversity and allows for adaptation, asexual reproduction can result in rapid population growth and the ability to colonize new habitats efficiently.
Sexual Reproduction in Plants
Sexual reproduction in plants is a complex process that involves the fusion of male and female reproductive structures to produce offspring. The key aspects of sexual reproduction in plants:
- Flower Formation: Many plants have flowers, which are specialized reproductive structures. Flowers contain male reproductive organs called stamens, which produce pollen, and female reproductive organs called pistils, which include the stigma, style, and ovary.
- Pollination: Pollination is the transfer of pollen from the male reproductive organs (anther) to the female reproductive organs (stigma). This can occur through various mechanisms, including wind, water, or animal pollinators such as bees, butterflies, birds, or bats.
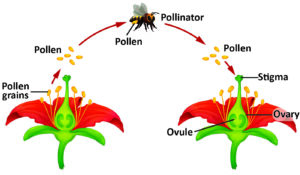
- Fertilization: Once pollen reaches the stigma, it germinates and grows a tube down the style to reach the ovary. This process is called pollen tube growth. The pollen tube delivers sperm cells to the ovary, where fertilization takes place. Fertilization involves the fusion of a sperm cell with an egg cell in the ovule, forming a zygote.
- Seed Development: After fertilization, the zygote develops into an embryo within the ovule. The ovule then develops into a seed, containing the embryo, endosperm (nutrient storage), and seed coat. The seed is dispersed from the parent plant and can germinate under favourable conditions to grow into a new plant.
- Genetic Variation: Sexual reproduction in plants leads to genetic diversity. The fusion of genetic material from two parent plants during fertilization results in offspring with a unique combination of traits. This genetic variation contributes to the adaptability and evolution of plant populations.
- Self-Pollination and Cross-Pollination: Plants can exhibit both self-pollination and cross-pollination. Self-pollination occurs when pollen from the same plant or flower fertilizes the ovule. Cross-pollination, on the other hand, involves the transfer of pollen between different plants, promoting genetic diversity.
Sexual reproduction in plants allows for genetic variation, which can enhance the survival and adaptation of plant populations to changing environmental conditions. It also facilitates the production of seeds, ensuring the dispersal and propagation of plant species.
Asexual reproduction in plants
Asexual reproduction in plants is a mode of reproduction that does not involve the fusion of gametes or the involvement of a mate. Instead, new individuals are produced from a single-parent plant, often through the use of vegetative structures. The key aspects of asexual reproduction in plants:
- Vegetative Propagation: Asexual reproduction in plants commonly occurs through vegetative propagation. This involves the growth and development of specialized plant structures that can give rise to new individuals. Examples include:
- Runners or Stolons: These are horizontal stems that grow above the ground, producing new plantlets at the nodes. Examples include strawberry plants.
- Rhizomes: Underground stems that send out roots and shoots, producing new plants. Examples include bamboo and ginger.
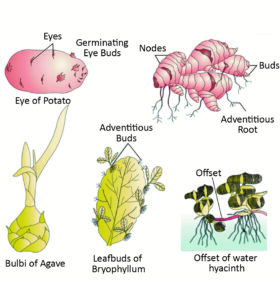
- Bulbs: Underground storage structures consisting of modified leaves. They produce new plants from buds called bulbils. Examples include onions and tulips.
- Tubers: Enlarged underground structures that store nutrients and can give rise to new plants. Examples include potatoes.
- Adventitious Plantlets: Some plants produce adventitious plantlets, which are miniature versions of the parent plant that develop on specialized structures. These plantlets can detach and grow into independent individuals. Examples include plantlets formed on the leaves of certain succulent plants like Bryophyllum.
- Apomixis: Apomixis is a type of asexual reproduction in which plants produce seeds without the process of fertilization. The seeds develop from the ovule without the involvement of pollination or the fusion of gametes. This allows for the production of offspring that are genetically identical to the parent plant.
- Fragmentation: In fragmentation, a plant breaks into pieces, and each fragment has the ability to develop into a new individual. This can occur naturally due to environmental factors or through intentional human intervention.
Asexual reproduction in plants allows for the rapid production of offspring without the need for a mate, ensuring the efficient colonization of new habitats. It results in the production of genetically identical or nearly identical offspring, preserving the traits of the parent plant.
While asexual reproduction lacks the genetic variation seen in sexual reproduction, it can be advantageous in stable environments or for plants that are well-adapted to their surroundings.
Sexual reproduction in animals
Sexual reproduction in animals is a process in which two individuals of the same species come together to produce offspring. It involves the fusion of specialized reproductive cells called gametes, typically a sperm cell from the male and an egg cell from the female. The key aspects of sexual reproduction in animals:
- Gamete Production: Animals have separate sexes, with individuals being either male or female. Males produce sperm cells, while females produce egg cells. These gametes contain half the number of chromosomes as the parent organism.
- Mating: Sexual reproduction in animals involves the mating of two individuals. Mating can occur through various mechanisms, such as courtship rituals, physical interactions, or external fertilization in aquatic environments.
- Fertilization: During mating, the male deposits sperm cells into the female reproductive system. Fertilization occurs when a sperm cell successfully penetrates and fuses with the egg cell, combining its genetic material. This fusion forms a zygote, which is the initial cell of the new individual.
- Embryo Development: The zygote undergoes a series of divisions and develops into an embryo. The embryo receives nourishment and protection within the female’s body or in specialized structures like eggs or nests.
- Birth or Hatching: After a period of development, the embryo is born or hatches from an egg, depending on the species. The offspring are then independent and begin their own life cycle.
Asexual Reproduction in Animals
Asexual reproduction in animals is a mode of reproduction that involves the production of offspring without the involvement of gametes or a mate. Unlike sexual reproduction, which requires the fusion of sperm and egg cells, asexual reproduction relies on other mechanisms to generate new individuals. The key aspects of asexual reproduction in animals:
- Budding: In budding, a new individual develops as an outgrowth or bud from the parent organism. The bud eventually separates from the parent and becomes an independent organism. Examples of animals that reproduce through budding include certain types of corals and hydra.
- Fission: Fission involves the splitting of the parent organism into two or more parts, with each part developing into a separate individual. This process can occur longitudinally or transversely. Some types of flatworms and sea anemones reproduce through fission.
- Fragmentation and Regeneration: Certain animals can regenerate from fragmented body parts. When an organism breaks into pieces, each fragment can regenerate and develop into a complete organism. This is observed in species such as starfish and planarians.
- Parthenogenesis: Parthenogenesis is the development of an embryo from an unfertilized egg. In this process, the female organism produces offspring without mating with a male. Parthenogenesis occurs in various animal groups, including some insects, reptiles, and fish.
Asexual reproduction in animals allows for rapid population growth and colonization of new habitats without the need to find a mate. It results in the production of genetically identical or nearly identical offspring, preserving the traits of the parent organism.
While asexual reproduction lacks the genetic variation seen in sexual reproduction, it can be advantageous in stable environments or for animals well-adapted to their surroundings. However, sexual reproduction is generally more common in the animal kingdom due to its potential for generating genetic diversity and adaptation to changing environments.
In conclusion, the study of inheritance and reproduction is essential for understanding the mechanisms by which traits and genetic information are passed down from one generation to the next. The chromosomal theory of inheritance provides a framework to explain how chromosomes, composed of genes, carry and transmit genetic material. Through sexual reproduction, organisms can introduce genetic diversity, promoting adaptation and evolution. The process of reproduction, whether sexual or asexual, ensures the continuity and survival of species.
Additionally, advancements in genetic research and technologies, such as gene therapy and genome sequencing projects, offer new possibilities for understanding and treating genetic disorders. The exploration of reproduction and inheritance continues to unveil the intricacies of life’s fundamental processes and paves the way for advancements in various fields, including medicine, agriculture, and conservation. As we deepen our knowledge in these areas, we gain insights into the remarkable complexity and interconnectedness of life on our planet.
Notes and References
- https://ncert.nic.in/ncerts/l/jesc109.pdf
- https://kitabcd.org/9th/notes-class-9-science-chapter-16-heredity-and-variations-maharashtra-board/
- https://www.thehindu.com/sci-tech/sequencing-indian-genes/article29865310.ece
- https://www.britannica.com/science/Mendelian-inheritance
- https://bioprinciples.biosci.gatech.edu/module-4-genes-and-genomes/4-4-linkage-sex-linkage-and-pedigree-analysis/
Blood
Introduction
Blood is a specialized bodily fluid that comprises several key components such as plasma, red blood cells, white blood cells, and platelets. Its primary functions encompass various vital roles, such as:
- Transporting oxygen and nutrients to the lungs and tissues;
- facilitating the formation of blood clots to prevent excessive blood loss;
- carrying cells and antibodies that combat infections; and
- delivering waste products to the kidneys and liver for filtration and cleansing, and regulating body temperature.
The blood that circulates through the veins, arteries, and capillaries is referred to as whole blood, which constitutes roughly 55 per cent plasma and 45 per cent blood cells. Blood accounts for approximately 7 to 8 per cent of an individual’s total body weight, with an average-sized man having around 12 pints and an average-sized woman having approximately nine pints of blood.
Components of Blood and Their Importance
Plasma
Plasma, the fluid component of blood, consists of a blend of water, sugar, fat, protein, and salts. Its primary function is to facilitate the transportation of blood cells, along with essential nutrients, waste products, antibodies, clotting proteins, chemical messengers (such as hormones), and proteins that aid in maintaining the body’s fluid balance.
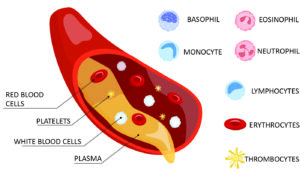
(Source: https://www.physio-pedia.com/Blood_Physiology)
Red Blood Cells (Erythrocytes or RBCs)
Distinguished by their vibrant red color, red blood cells constitute the most abundant cell type in the bloodstream, comprising approximately 40 to 45 percent of its volume. These cells possess a biconcave disk shape with a flattened center, resembling a donut with shallow bowl-like indentations on both faces.
The production of red blood cells is regulated by erythropoietin, a hormone primarily synthesized by the kidneys. Unlike many other cell types, red blood cells lack a nucleus and can easily alter their shape, enabling them to navigate through the diverse blood vessels within the body. However, the absence of a nucleus grants them greater flexibility while imposing limitations on their lifespan. As red blood cells traverse the smallest blood vessels, their membranes may be subjected to damage, depleting their energy reserves. On average, a red blood cell survives for only about 120 days.
Red blood cells are equipped with a unique protein called haemoglobin, which plays a crucial role in transporting oxygen from the lungs to the body’s tissues and facilitating the return of carbon dioxide from the tissues back to the lungs for exhalation. The distinctive red hue of blood arises from the abundance of red blood cells, which derive their color from haemoglobin. The hematocrit, a widely used measure of red blood cell levels, represents the percentage of total blood volume occupied by red blood cells.
White Blood Cells (leukocytes or WBCs)
White blood cells play a crucial role in safeguarding the body against infections. They are present in much smaller numbers compared to red blood cells, constituting approximately 1 per cent of the total blood volume.
Among the various types of white blood cells, the most common is the neutrophil, which acts as an immediate response cell and accounts for 55 to 70 percent of the total white blood cell count. Neutrophils have a short lifespan of less than a day, necessitating the continuous production of new neutrophils by the bone marrow to ensure ongoing protection against infections. Transfusing neutrophils is generally ineffective since they do not persist in the body for extended periods.
Another significant type of white blood cell is the lymphocyte. There are two main subtypes of lymphocytes. T lymphocytes aid in regulating the function of other immune cells and directly target infected cells and tumours. On the other hand, B lymphocytes produce antibodies, specialized proteins that specifically recognize and target bacteria, viruses, and other foreign substances.
Platelets (thrombocytes)
Platelets differ from red and white blood cells as they are not complete cells but rather small cell fragments. Their primary function is to aid in the process of blood clotting, also known as coagulation. When an injury occurs, platelets gather at the site, adhere to the lining of the injured blood vessel, and create a platform that facilitates blood coagulation. This process culminates in the formation of a fibrin clot, which covers the wound, prevents blood leakage, and serves as a framework for the development of new tissue, thus promoting the healing process.
Abnormally high platelet counts can lead to excessive clotting, potentially resulting in strokes and heart attacks. Fortunately, advancements in antiplatelet therapies have provided treatments to mitigate these life-threatening events. Conversely, lower than normal platelet counts can lead to significant bleeding.
Complete Blood Count (CBC)
The Complete Blood Count (CBC) test provides valuable information to your doctor regarding the composition of your blood, specifically the types and quantities of cells present, including red blood cells with their hematocrit or hemoglobin levels, white blood cells, and platelets. By analyzing the results of a CBC, various conditions such as anemia, infections, and other disorders can be diagnosed. In addition, the platelet count and plasma clotting tests such as prothrombin time, partial thromboplastin time, and thrombin time are utilized to assess potential bleeding and clotting disorders.
| Important Information |
| Neutrophils
Neutrophils, a type of white blood cell (WBC), are produced in the bone marrow and make up approximately 50% of the total WBC count. Each day, the bone marrow generates about 100 billion neutrophil cells. These cells are recognized as the initial line of defense in the immune system, being the first immune cells to respond to infections. Their primary role is to combat pathogens by migrating to infection sites and effectively identifying and eliminating bacteria and viruses. Furthermore, neutrophils play a crucial role in immune system coordination by releasing signals that alert other immune cells. Monocytes Monocytes make up approximately 5 to 12% of the total white blood cell (WBC) count. They are recognized as the “garbage trucks” of the immune system due to their crucial role in removing dead cells and promoting tissue regeneration. Eosinophils Eosinophils make up less than 5% of the total white blood cells (WBCs). They are predominantly found in significant quantities in the digestive system. Eosinophils have a vital function in combating invading bacteria and parasites, particularly those such as worms. Basophils Basophils account for approximately 1% of the total white blood cell count. These cells are involved in the development of asthma. They stimulate the release of histamine, which contributes to the inflammation and constriction of the airways that occur in asthma. |
Blood Vessels
Blood vessels serve as conduits that transport blood throughout the entire body, forming a closed loop that starts and finishes at the heart. Collectively, the heart, blood vessels, and associated structures constitute the circulatory system. Remarkably, the human body boasts approximately 60,000 miles of intricate blood vessels. There are three types of blood vessels:
- Arteries carry blood away from your heart.
- Veins carry blood back toward your heart.
- Capillaries, the smallest blood vessels, connect arteries and veins.
The flow of Blood in the Human Body
- Veins: Bring blood to the right side of the heart.
- Pulmonary arteries: Carry blood to the lungs for oxygenation.
- Pulmonary veins: Transport oxygen-rich blood to the left side of the heart.
- Aorta: A main artery that carries blood from the left side of the heart to the body through various arterial branches.
- Capillaries: Thin-walled vessels allow the exchange of oxygen, nutrients, carbon dioxide, and waste products with tissue cells.
- Veins: Return blood back to the heart, restarting the process.
Purpose of blood vessels
Blood vessels play a crucial role in delivering blood to organs and tissues throughout the body, providing them with essential oxygen and nutrients while removing waste products and carbon dioxide. Each type of blood vessel serves a distinct function:
- Arteries: Strong and muscular vessels that transport oxygen-rich blood from the heart to organs, experiencing high pressure but carrying a smaller blood volume.
- Arterioles: Smaller branches of arteries that regulate blood pressure by adjusting their size.
- Capillaries: Tiny vessels with thin walls, facilitate the exchange of oxygen, nutrients, and waste products between blood and organs/tissues.
- Venules: Small vessels receiving blood from capillaries and gradually increasing in size.
- Veins: Transport deoxygenated blood back to the heart at lower pressure but with a larger blood volume. They have thin walls and often feature valves to maintain one-way blood flow. The majority of the body’s blood is found in veins.
Location of Blood Vessels
Blood vessels are distributed throughout the entirety of the body. The principal artery, known as the aorta, originates from the left side of the heart and extends downward, passing through the chest, diaphragm, and abdomen. Along its course, the aorta branches out into numerous arteries. Near the pelvis, the aorta further divides into two arteries that supply blood to the lower body and legs.
The primary vein in the body is called the vena cava. The superior vena cava is located in the upper right part of the chest and carries blood from the head, neck, arms, and chest back to the heart. On the other hand, the inferior vena cava is situated near the right side of the diaphragm, responsible for returning blood from the legs, feet, abdomen, and pelvis back to the heart.
Constituents of the blood vessels
Blood vessels have three layers of tissue:
- Tunica intima: The inner layer that encloses circulating blood, responsible for regulating blood pressure, preventing clotting, and safeguarding against toxins. It ensures the smooth flow of blood.
- Media: The middle layer consisting of elastic fibers that facilitate unidirectional blood flow. It aids in vessel expansion and contraction, contributing to their flexibility.
- Adventitia: The outer layer housing nerves and small vessels. It delivers oxygen and nutrients to cells, removes waste products, and provides structural support to blood vessels.
Conditions and disorders of the blood vessels
A wide range of problems can affect your blood vessels, including:
- Aneurysm: A bulge that develops in a weakened or damaged area of an artery, which can occur anywhere in the body. If an aneurysm ruptures, it can result in severe internal bleeding that poses a life-threatening situation.
- Arterial diseases: This category includes coronary artery disease, carotid artery disease, and peripheral artery disease (PAD). These conditions lead to the narrowing of arteries, often caused by the buildup of plaque known as atherosclerosis.
- Atherosclerosis: The accumulation of plaque, consisting of cholesterol, fat, and other substances, within the arteries. Atherosclerosis increases the risk of heart attacks and strokes.
- Blood clots: Formations of clumps within veins or arteries that obstruct blood flow. Blood clots can lead to conditions such as deep vein thrombosis (DVT), pulmonary embolism, stroke, or blockage of an artery.
- High blood pressure (hypertension): A condition characterized by excessive force against the artery walls, often resulting from underlying factors.
- Raynaud’s disease: A condition causing the constriction of arteries that supply blood to the skin, particularly in response to cold temperatures.
- Varicose veins: Enlarged and twisted veins that commonly occur in the legs or feet.
- Vascular malformations: Abnormal clusters or connections between blood vessels, with conditions like arteriovenous malformations often present from birth (congenital).
- Vasculitis: Inflammation of blood vessel walls, leading to thickening and narrowing, which hampers the smooth flow of blood.
Functions of Blood
Blood Is Fluid Connective Tissue
Blood consists of two main components: plasma and formed elements. Plasma constitutes approximately 55% of the blood composition, while the remaining 45% comprises the formed elements, which encompass red blood cells, white blood cells, and platelets. The presence of these cellular elements within the plasma classifies blood as a fluid connective tissue, distinguishing it from ordinary fluids. As such, blood stands as the sole fluid tissue in the human body.
Blood Provides the Body’s Cells with Oxygen and Removes Carbon Dioxide
Oxygen is taken up by blood from the air present in the lungs. Subsequently, blood carries this oxygen to cells across the entire body while simultaneously extracting waste carbon dioxide from these cells. In the lungs, carbon dioxide transfers from the blood to the air, eventually being exhaled.
Blood Transports Nutrients and Hormones
Blood plays a significant role in facilitating digestion and supporting the functions of the endocrine system. During the process of digestion, nutrients that have been broken down are absorbed into the bloodstream through the capillaries found in the villi of the small intestine. These essential nutrients include glucose, amino acids, vitamins, minerals, and fatty acids. Additionally, blood acts as a carrier for certain hormones that are produced by the glands of the endocrine system. These hormones are transported through the bloodstream to specific target organs and tissues, where they exert their regulatory effects.
Blood Regulates Body Temperature
Blood plays a vital role in the absorption and distribution of heat throughout the body, contributing to the maintenance of homeostasis. One of its functions is to regulate body temperature by either releasing or conserving warmth as needed. This process involves the dynamic response of blood vessels, which can expand or contract in response to external factors like bacteria, as well as internal changes in hormones and chemicals. By adjusting the diameter of blood vessels, blood flow and heat can be directed closer to or farther away from the skin surface, influencing the amount of heat that is lost from the body.
Platelets Clot Blood at Sites of Injury
In the event of a blood vessel tear, platelets and plasma proteins collaborate to prevent excessive blood loss. Platelets, also known as thrombocytes, aggregate and create a plug at the site of injury. Simultaneously, plasma proteins form fibrin threads, which contribute to the formation of a clot, finalizing the platelet plug. Together, these mechanisms help to staunch bleeding and facilitate the healing process.
Blood Brings Waste Products to the Kidneys and Liver
Blood serves as a carrier for waste substances, transporting them to the organs responsible for their elimination and processing. Renal arteries supply blood to the kidneys, where waste products like urea, uric acid, and creatinine are filtered out of the blood plasma and directed into the ureters. The blood then exits the kidneys through the renal veins. Additionally, the liver plays a crucial role in removing toxins from the blood. During the process of digestion, the liver cleanses the blood, extracting vitamins and enriching it before redistributing it to the rest of the body. These mechanisms ensure the effective elimination of waste substances and contribute to overall bodily functioning.
Red Blood Cells Are the Most Numerous Living Cells in Blood
Blood is composed of approximately 55% plasma and 45% formed elements. Among the formed elements, red blood cells, also known as erythrocytes, constitute the majority. Their main role is to transport oxygen from the lungs to the body’s cells. Red blood cells possess a distinctive disc-shaped structure with a flattened center, giving them a biconcave shape. This unique shape allows for flexibility and efficient oxygen-carrying capacity, enabling them to navigate through the narrowest blood vessels and effectively deliver oxygen to tissues throughout the body.
White Blood Cells Protect the Body from Pathogens
White blood cells, or leukocytes, play a vital role in combating diseases and infections within the body. Although they constitute only 1% of the total blood volume, their numbers increase during times of infection or inflammation. There are five major types of white blood cells: neutrophils, eosinophils, basophils, lymphocytes, and monocytes. Among these, neutrophils are the most prevalent, accounting for approximately 60% to 70% of all white blood cells. Each type of white blood cell possesses unique functions and contributes to the body’s immune response in different ways. Together, they form a crucial defense mechanism against pathogens and maintain overall health.
Origin of Blood Cells
Blood cells are derived from hematopoietic stem cells, which undergo a controlled process called hematopoiesis in the bone marrow. Hematopoietic stem cells possess the ability to differentiate into different types of blood cells, including red blood cells, white blood cells, and platelets. These versatile stem cells can be found in the circulating blood and bone marrow of individuals of all ages, as well as in the umbilical cords of newborns. Stem cells obtained from these sources have been utilized in the treatment of various diseases such as leukemia, lymphoma, bone marrow failure, and immune disorders. The therapeutic potential of these stem cells offers promising prospects for medical interventions and regenerative therapies.
Various types of Blood Tests
- Complete blood count (CBC): This test measures the concentration of red blood cells, white blood cells, and platelets in the blood. Automated cell counters are commonly used to perform this analysis.
- Blood smear: A technique where drops of blood are spread thinly on a microscope slide and examined by laboratory experts. Blood smears are useful in identifying various blood conditions such as leukemia, anemia, and malaria.
- Blood typing: A test conducted to determine the compatibility of blood before a transfusion. It involves identifying the major blood types (A, B, AB, and O) based on the presence of specific protein markers (antigens) on the surface of red blood cells.
- Coombs test: This blood test aims to detect antibodies that may attach to and destroy red blood cells. It is commonly performed in pregnant women and individuals with anemia.
- Blood culture: This test is used to identify the presence of infections in the bloodstream. By collecting a sample of blood, the culture allows bacteria or other organisms to grow and be identified.
- Mixing study: This blood test is conducted to determine the cause of abnormal blood clotting or increased “thinness.” The patient’s blood is mixed with normal blood in a tube, and the resulting properties of the mixture can provide valuable diagnostic information.
- Bone marrow biopsy: In this procedure, a thick needle is inserted into a large bone, typically the hip, to extract a sample of bone marrow for further testing and analysis. Bone marrow biopsies are helpful in evaluating various conditions related to the bone marrow.
| World Blood Donor Day |
| World Blood Donor Day, observed on 14 June each year, serves several important purposes:
Increasing awareness: The day aims to raise global awareness about the ongoing need for safe blood and blood products for transfusion. This helps educate the public about the importance of donating blood and its impact on saving lives. Recognizing voluntary donors: It highlights the invaluable contribution of voluntary, unpaid blood donors to national health systems. By acknowledging their selfless act, the day emphasizes the role of individuals in providing life-saving blood for those in need. Strengthening blood donor programs: World Blood Donor Day supports national blood transfusion services, blood donor organizations, and other non-governmental organizations in enhancing and expanding their voluntary blood donor programs. It encourages the development of national and local campaigns to promote |
Types of Blood Groups
There are four primary blood groups, namely A, B, AB, and O, which are determined by the genetic inheritance from parents. Each blood group can further be categorized as RhD positive or RhD negative, resulting in a total of eight blood groups. Blood consists of red blood cells, white blood cells, platelets, and plasma, a liquid component. The identification of blood groups relies on the presence of antibodies and antigens in the blood. Antibodies, proteins found in plasma, play a role in the body’s immune response by recognizing and alerting the immune system to foreign substances, such as germs, leading to their elimination. On the other hand, antigens are protein molecules located on the surface of red blood cells, distinguishing different blood groups.
| Blood Group | Antigens (in red blood cells) | Antibodies (in plasma) |
| A | A | Anti-B |
| B | B | Anti-A |
| O | nil | Anti-A, Anti-B |
| AB | A, B | nil |
ABO system
There are 4 main blood groups defined by the ABO system:
- Blood group A – has A antigens on the red blood cells with anti-B antibodies in the plasma
- Blood group B – has B antigens with anti-A antibodies in the plasma
- Blood group O – has no antigens, but both anti-A and anti-B antibodies in the plasma
- Blood group AB – has both A and B antigens, but no antibodies
Rh System
Red blood cells sometimes have another antigen, a protein known as the RhD antigen. If this is present, your blood group is RhD positive. If it’s absent, your blood group is RhD negative. This means you can be 1 of 8 blood groups:
- A RhD positive (A+)
- A RhD negative (A-)
- B RhD positive (B+)
- B RhD negative (B-)
- RhD positive (O+)
- RhD negative (O-)
- AB RhD positive (AB+)
- AB RhD negative (AB-)
What is a Universal Blood Donor?
The O negative blood type is considered a universal donor because it can be used in transfusions for individuals with any blood type. This blood type is highly sought after by hospitals due to its versatility and essential role in emergency situations and transfusions for immune deficient infants. Type O blood, both positive and negative, is the most common blood type among Caucasians (45%), African-Americans (51%), and Hispanics (57%). The prevalence of type O blood in diverse populations is particularly significant as it helps meet the constant demand for blood supply.
Both O negative and O positive blood types are in high demand, with only 7% of the population having O negative blood. The need for O negative blood is especially critical because it is frequently used in emergency cases. O positive blood is also in high demand as it is the most prevalent blood type, found in 37% of the population. While individuals with Type O negative blood can serve as universal red cell donors, those with Type AB blood are considered universal plasma donors. Understanding the importance of blood types and their availability is crucial for maintaining a sufficient and diverse blood supply to meet the ongoing needs of patients.
Blood Disorders
Hematology
Hematology is a field of study focused on understanding the intricacies of blood in both healthy and diseased states. It encompasses various aspects related to red blood cells, white blood cells, platelets, blood vessels, bone marrow, lymph nodes, spleen, and the proteins involved in the processes of bleeding and clotting, known as hemostasis and thrombosis. A hematologist is a medical doctor who specializes in this area and applies their expertise to diagnose and treat patients with blood disorders and conditions.
Disorders associated with Blood
Anemia
Anemia is a condition characterized by insufficient red blood cells or inadequate levels of hemoglobin, which is essential for carrying oxygen from the lungs to various tissues in the body. Hemoglobin is a protein found in red blood cells that binds with oxygen. The production of healthy red blood cells relies on the presence of vitamins B12 and folate. There are several causes of anemia, including blood loss, the destruction of red blood cells, and impaired blood production due to factors such as impaired bone marrow function or deficiencies in iron, vitamin B12, or folate.
Role of Red Blood Cells in Anemia
Red blood cells play a vital role in transporting oxygen throughout the body by carrying hemoglobin, an iron-rich protein that binds to oxygen in the lungs. When there is a deficiency of red blood cells or when they do not function effectively, a condition known as anemia occurs. Anemia is typically diagnosed through a blood test that measures hemoglobin levels. In men, anemia is identified when the hemoglobin value is less than 13.5 gm/dl, while in women, it is less than 12.0 gm/dl. Normal hemoglobin values for children vary depending on their age.
Common Types of Anemia
- Iron-deficiency anemia is the predominant form of anemia, resulting from insufficient iron levels in the body. It is commonly caused by blood loss or impaired iron absorption. Pregnancy and gastric bypass surgery can lead to iron deficiency due to increased iron demands or reduced absorption.
- Vitamin-deficiency anemia occurs when there are low levels of vitamin B12 or folate (folic acid), usually due to inadequate dietary intake. Pernicious anemia is a condition characterized by the inability to absorb vitamin B12 in the gastrointestinal tract.
- Anemia during pregnancy has specific risk factors and symptoms associated with it.
- Aplastic anemia is a rare disorder where the bone marrow fails to produce enough blood cells (red blood cells, white blood cells, and platelets). This can occur due to destruction or deficiency of blood-forming stem cells, often as a result of the immune system attacking these cells. However, the few blood cells that are produced in the bone marrow are normal. Aplastic anemia can also be caused by viral infections, ionizing radiation, or exposure to toxic chemicals or drugs.
- Hemolytic anemia occurs when red blood cells are prematurely broken down in the bloodstream or spleen. It can be caused by various factors, including mechanical issues like leaky heart valves or aneurysms, infections, autoimmune disorders, or inherited abnormalities affecting the structure or function of red blood cells. Examples of inherited hemolytic anemias include certain types of thalassemia and deficiencies in enzymes like glucose-6-phosphate dehydrogenase. The treatment for hemolytic anemia depends on the underlying cause.
- Sickle cell anemia is an inherited form of hemolytic anemia in which the abnormal hemoglobin protein causes red blood cells to become rigid and obstruct blood flow in small blood vessels.
- Anemia can also be caused by other diseases that affect the body’s ability to produce red blood cells. For instance, kidney disease can lead to anemia because the kidneys do not produce enough erythropoietin, the hormone responsible for stimulating red blood cell production in the bone marrow. Additionally, chemotherapy used in cancer treatment can impair the production of new red blood cells, resulting in anemia.
Bleeding Disorders
Bleeding disorders encompass a range of conditions that occur when blood fails to clot properly. In the normal clotting process, platelets, a type of blood cell, aggregate and form a plug at the site of a damaged blood vessel. Clotting factors, proteins in the blood, then interact to create a fibrin clot, a gel-like structure that stabilizes the platelets, promotes healing, and prevents excessive blood loss. While excessive clotting can lead to health issues like heart attacks and strokes, the inability to form clots can be equally hazardous, resulting in excessive bleeding. Bleeding disorders can stem from deficiencies or abnormalities in platelets, clotting proteins, or blood vessels.
Hemophilia is a well-known inherited bleeding disorder, albeit rare, primarily affecting males. Von Willebrand disease is more prevalent and the most common inherited bleeding disorder in the United States, caused by deficiencies in clotting proteins. Von Willebrand disease can affect both males and females. Platelet disorders, typically acquired rather than inherited, represent the most frequent cause of bleeding disorders.
In summary, bleeding disorders encompass a range of conditions where blood clotting is impaired, resulting in abnormal or inadequate clot formation. Hemophilia and von Willebrand disease are notable examples, with hemophilia affecting mainly males and von Willebrand disease affecting both genders. Platelet disorders, often acquired, are the most common cause of bleeding disorders.
What Is Hemophilia and How Is It Treated?
Hemophilia is a rare inherited bleeding disorder characterized by the deficiency of clotting factors in the blood. The severity of the condition varies depending on the amount of clotting factor present. Hemophilia is classified into two types: type A, caused by a lack of factor VIII clotting factor, and type B, caused by a deficiency of factor IX clotting factor. The genetic defect responsible for hemophilia is located on the X chromosome, and since women have two X chromosomes, they can be carriers of the defective gene and pass it on to their sons. Female carriers may exhibit varying symptoms due to random inactivation of their X chromosomes. Men, who have one X and one Y chromosome, will have hemophilia if their X chromosome carries the defective gene.
Insufficient clotting factor in hemophilia leads to a higher risk of excessive bleeding following cuts or injuries. Individuals with hemophilia are also prone to internal bleeding, which can result in joint, organ, and tissue damage over time.
Historically, hemophilia treatment involved transfusions of factor VIII derived from donor blood. However, in the 1980s, it was discovered that these products carried blood-borne viruses like hepatitis and HIV. Advances in screening techniques and the development of synthetic blood factors through gene cloning have significantly improved treatment. Today, factor-replacement therapies produced in laboratories offer pure and safer alternatives for managing hemophilia.
What Is von Willebrand Disease and How Is It Treated?
Von Willebrand disease is an inherited disorder characterized by the absence or malfunctioning of von Willebrand factor, a protein essential for blood clotting and carrying another clotting protein called factor VIII. It is a condition that can affect both males and females, with women experiencing heightened symptoms during menstruation. Von Willebrand disease is categorized into three types (Types 1, 2, and 3) based on the levels of von Willebrand factor and factor VIII activity in the blood. Type 1 is the most common and mildest form, while Type 3 is the least common and most severe.
Early diagnosis is crucial in managing von Willebrand disease, and with appropriate care, individuals can lead normal, active lives. Mild cases may not require treatment, but it is important to avoid medications like aspirin and ibuprofen that can increase the risk of bleeding without medical guidance. More severe cases can be managed with medications that raise the levels of von Willebrand factor or through infusions of blood factor concentrates. Individuals with von Willebrand disease should consult with their healthcare providers before undergoing surgery, dental procedures, or giving birth to ensure appropriate precautions are taken to prevent excessive bleeding. Referral to a hematologist, a specialist in blood disorders, may be recommended for comprehensive management.
What is Blood Clot?
Blood clotting, also known as coagulation, is a vital process that prevents excessive bleeding when a blood vessel is damaged. It involves the collaboration of platelets and plasma proteins to form a clot at the site of injury, effectively stopping the bleeding. Normally, the body naturally dissolves the clot once healing has occurred. However, there are instances where clots form inside blood vessels without apparent injury or fail to dissolve on their own, leading to potential complications that require accurate diagnosis and appropriate treatment.
Clots can develop in veins or arteries, which are integral components of the body’s circulatory system, although they have different functions. Veins are responsible for carrying deoxygenated blood back to the heart from organs, operating under low pressure. When an abnormal clot forms in a vein, it can impede blood flow, leading to pain and swelling as blood accumulates behind the clot. Deep vein thrombosis (DVT) is a type of clot that typically occurs in a major leg vein but can also affect the arms, pelvis, or other large veins in the body. In certain cases, a clot in a vein may dislodge and travel through the heart to the lungs, where it becomes lodged, obstructing proper blood flow. This is known as a pulmonary embolism (PE) and can be extremely hazardous.
Blood Cancer
Blood cancers are a group of diseases that impact the production and function of blood cells. They typically originate in the bone marrow, where blood cells are formed. Within the bone marrow, stem cells mature and differentiate into three types of blood cells: red blood cells, white blood cells, and platelets. In blood cancers, this normal process of blood cell development is disrupted by the uncontrolled growth of abnormal cells. These cancerous cells interfere with the normal functioning of the blood, compromising its ability to fight infections and prevent excessive bleeding. There are three primary types of blood cancers:
- Leukemia is a blood cancer characterized by the rapid proliferation of abnormal white blood cells. These abnormal cells are unable to perform their immune functions properly, and their excessive accumulation interferes with the production of normal red blood cells and platelets in the bone marrow.
- Lymphoma is a type of blood cancer that affects the lymphatic system, which plays a role in fluid balance and immune response. In lymphoma, abnormal lymphocytes, a type of white blood cell, undergo malignant changes and form cancerous lymphoma cells. These cells multiply and accumulate in lymph nodes and other tissues, impairing the normal functioning of the immune system.
- Myeloma is a cancer that specifically targets plasma cells, a type of white blood cell responsible for producing antibodies that help fight infections. In myeloma, malignant plasma cells inhibit the production of healthy antibodies, weakening the immune system and making the body more susceptible to infections and other complications.
Key Differences between Cancer cells and Normal cells
- Cancer cells keep dividing: Cancer cells have a disrupted cell cycle and continue to divide uncontrollably, disregarding signals from the body to stop dividing. Unlike normal cells, they do not undergo programmed cell death (apoptosis) when they are no longer needed.
- Cancer cells grow too rapidly to mature: Cancer cells grow rapidly and fail to mature into specialized cell types like normal cells do. This lack of maturation leads to the accumulation of immature cells with abnormal characteristics.
- Cancer cells may influence normal cells: Cancer cells can influence the behavior of normal cells, molecules, and blood vessels in their vicinity. They may release signals that recruit normal cells to support tumor growth, such as promoting the formation of new blood vessels (angiogenesis) to supply the tumor with nutrients and oxygen.
- Cancer cells trick the immune system: Cancer cells can evade the immune system’s surveillance and destruction. They may develop mechanisms to avoid recognition and attack by immune cells, allowing them to survive and continue growing.
- Cancer cells are invasive: Cancer cells can invade nearby tissues due to their uncontrolled growth and ability to ignore signals that regulate tissue boundaries. Malignant tumors have the potential to invade surrounding tissues and infiltrate different organs or body regions.
- Cancer cells may spread to other parts of the body: Cancer cells have the ability to spread to other parts of the body through a process called metastasis. They can detach from the primary tumor, enter the bloodstream or lymphatic system, and establish secondary tumors in distant organs or tissues. The secondary tumors are still identified based on their origin, such as metastatic lung cancer even if found in another location.
Various Blood Treatments
- Chemotherapy is a treatment method that involves using drugs to kill cancer cells. It is commonly used in the treatment of leukemia and lymphoma, where medications are administered to target and destroy cancer cells throughout the body.
- Blood transfusion is a procedure where donated blood is given to a recipient to replace blood loss or to increase the number of healthy blood cells. In the case of severe anemia or blood loss, red blood cells from a compatible donor are transfused to restore the patient’s blood volume and oxygen-carrying capacity.
- Platelet transfusion is a procedure in which platelets, a component of blood involved in clotting, are transfused to individuals with low platelet counts. It is typically performed when platelet levels are critically low and there is an increased risk of bleeding.
- Fresh frozen plasma (FFP) is the liquid portion of blood that contains clotting factors. It is separated from donated blood and frozen for storage. FFP transfusion is used to improve blood clotting and treat clotting disorders or excessive bleeding caused by clotting problems.
- Cryoprecipitate is a blood product derived from plasma that contains concentrated amounts of specific clotting proteins. It is used to replace specific clotting factors in individuals with low levels of those proteins, such as patients with hemophilia.
- Anticoagulation involves the use of medications, such as heparin, enoxaparin (Lovenox), or warfarin (Coumadin), to prevent blood clotting in individuals at high risk of developing blood clots. These medications help thin the blood and reduce the risk of clot formation.
- Antiplatelet drugs, such as aspirin and clopidogrel (Plavix), interfere with platelet function and help prevent the formation of blood clots. They are commonly used to reduce the risk of heart attacks, strokes, and other clot-related conditions.
- Antibiotics are medications used to treat infections caused by bacteria or parasites. In the context of blood infections, antibiotics can be administered to combat the organisms responsible for the infection and restore health.
- Erythropoietin is a hormone naturally produced by the kidneys that stimulates the production of red blood cells in the bone marrow. Synthetic forms of erythropoietin can be administered to individuals with certain types of anemia to increase red blood cell production and improve symptoms.
- Bloodletting is a therapeutic procedure in which a controlled removal of blood is performed in individuals with conditions characterized by excess blood volume, such as hemochromatosis (excessive iron absorption) or polycythemia (excessive red blood cell production). The aim is to reduce blood levels and alleviate associated complications. However, this practice is now less common and reserved for specific cases under medical supervision.
Current Development
Risk of rare blood-clotting condition after covid-19 vaccination
A recent study published in The BMJ highlights the risk of developing a rare blood clotting condition, thrombosis with thrombocytopenia syndrome (TTS), following COVID-19 vaccination. The research analyzed health data from several European countries and the US, revealing a slightly increased risk of TTS after receiving the first dose of the Oxford-AstraZeneca vaccine. Additionally, there was a trend towards an increased risk after the Janssen/Johnson & Johnson vaccine compared to the Pfizer-BioNTech vaccine. While the researchers emphasize the rarity of this syndrome, they suggest considering these observed risks in future immunization campaigns and vaccine development.
Thrombosis with thrombocytopenia syndrome (TTS) is an uncommon condition characterized by blood clotting and low blood platelet counts. It is distinct from other clotting disorders such as deep vein thrombosis or pulmonary embolism. TTS is currently being investigated as a potential rare side effect of adenovirus-based COVID-19 vaccines that use weakened viruses to trigger an immune response. However, comparative safety data among different vaccine types remain inconclusive.
To address the knowledge gap surrounding TTS and its association with COVID-19 vaccines, an international team of researchers conducted a study comparing the risk of TTS and thromboembolic events between adenovirus-based vaccines (Oxford-AstraZeneca and Janssen/Johnson & Johnson) and mRNA-based vaccines (Pfizer-BioNTech and Moderna). The study analyzed health data from over 10 million adults in several countries who received at least one dose of a COVID-19 vaccine between December 2020 and mid-2021. Factors such as age, sex, pre-existing conditions, and medication use were considered to minimize potential errors.
The study focused on comparing rates of thrombosis and thrombosis with thrombocytopenia within 28 days after vaccination. Participants who received adenovirus-based vaccines were matched with those who received mRNA-based vaccines based on age, sex, and other relevant factors. The findings provide insights into the relative risks associated with different vaccine types and contribute to understanding the safety profiles of adenovirus-based and mRNA-based COVID-19 vaccines.
What is Thrombosis with thrombocytopenia syndrome (TTS)?
- Thrombosis with thrombocytopenia syndrome (TTS), also known as vaccine-induced immune thrombotic thrombocytopenia (VITT), is an extremely rare and distinct syndrome characterized by the simultaneous occurrence of blood clots (thrombosis) and low platelet counts (thrombocytopenia).
- Thrombosis refers to the formation of abnormal blood clots that hinder the normal flow of blood throughout the body, while thrombocytopenia indicates a deficiency of platelets in the blood, which are crucial for clotting and preventing excessive bleeding.
- TTS poses the risk of both clotting and bleeding problems due to the combined effects of clots and low platelet levels. Various factors can contribute to thrombocytopenia, including medications, cancer, certain cancer treatments, pregnancy, infection, an enlarged spleen, and, in rare instances, the consumption of quinine in tonic water.
E-cigarettes linked with blood vessel damage
Recent studies have highlighted the potential health risks associated with electronic cigarette (e-cigarette) use, popularly known as vaping, which was initially considered a safer alternative to traditional cigarette smoking. To delve deeper into the effects of e-cigarette use on the cardiovascular system, a team of researchers led by Dr. Matthew Springer from the University of California, San Francisco conducted a study involving 120 adults aged 21 to 50 who were in good overall health and had no known heart issues. Out of the participants, 42 were regular e-cigarette users, 28 were conventional cigarette smokers, and 50 did not use either product.
The researchers examined blood samples from all the volunteers to assess changes in chemicals related to blood flow and used ultrasound to measure blood vessel function in a subset of individuals from each group. The findings, published in Arteriosclerosis, Thrombosis, and Vascular Biology, revealed that both cigarette smokers and e-cigarette users exhibited reduced ability of blood vessels to expand compared to non-smokers, even after accounting for age, sex, and other heart function measurements.
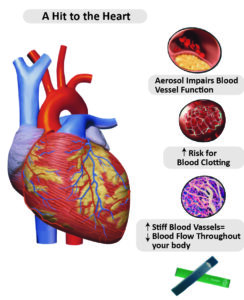
(Source: https://med.stanford.edu/visit/the-details/HealthEffects.html)
Further investigations involved exposing blood-vessel cells cultured in a lab to the participants’ blood serum. The serum obtained from smokers or e-cigarette users resulted in lower release of nitric oxide, a compound essential for regulating normal blood flow in vessels, compared to serum from non-users. Additionally, serum from e-cigarette users caused increased permeability or leakage in the cells, indicating impaired blood vessel function. Surprisingly, when cultured cells were directly exposed to isolated chemicals from cigarettes or e-cigarettes, there were no changes in nitric oxide production or permeability, suggesting that the observed cell damage was driven by the body’s response to chemical exposure rather than the chemicals themselves.
Both smokers and e-cigarette users exhibited signs of heightened inflammation and increased risk of blood clots, but the specific molecules affected differed between the two groups. Further experiments indicated that cigarette and e-cigarette use influenced cells through distinct mechanisms. These findings shed light on the potential adverse effects of e-cigarette use on cardiovascular health and emphasize the need for further research to better understand the risks associated with these products.
Blood-based biomarkers
A recent study supported by the National Institutes of Health (NIH) has discovered that specific biomarkers present in the blood shortly after a traumatic brain injury (TBI) can effectively predict the likelihood of death or severe disability six months later. Published in Lancet Neurology, the study focused on measuring the levels of glial fibrillary acidic protein (GFAP) and ubiquitin carboxy-terminal hydrolase L1 (UCH-L1) in approximately 1,700 TBI patients. These proteins are found in glial cells and neurons, respectively. By analyzing these biomarkers, clinicians may gain more accurate insights into patient prognosis following a TBI.
| What is a Biomarker? |
| A biological molecule found in blood, other body fluids, or tissues that is a sign of a normal or abnormal process, or of a condition or disease. A biomarker may be used to see how well the body responds to a treatment for a disease or condition. Also called molecular marker and signature molecule. |
Participants were recruited from 18 high-level trauma centers across the United States, with over half of them having sustained TBIs from road traffic accidents. The study demonstrated that elevated levels of GFAP and UCH-L1 on the day of the injury were robust indicators of unfavorable outcomes, including death and conditions such as vegetative state or severe disability necessitating daily assistance. Patients with biomarker levels among the highest fifth faced the greatest risk of death within the first month following the TBI.
While GFAP and UCH-L1 are already used to assist in the detection of TBIs and guide decisions regarding brain imaging, this research suggests that they could also serve as valuable predictors of recovery, particularly in cases of moderate to severe TBI. The biomarkers improved the accuracy of existing prognostic models; however, they were not as effective in predicting incomplete recovery, characterized by moderate disability but the ability to live independently, at the six-month mark. Further studies are needed to validate these findings, but they indicate that blood-based biomarkers have the potential to enhance clinicians’ ability to forecast patient outcomes following a TBI.
Blood safety and availability
Key Data
- Out of the 118.5 million blood donations collected worldwide, 40% of these donations come from high-income countries, which are home to only 16% of the global population.
- In low-income countries, approximately 54% of blood transfusions are administered to children under the age of 5, whereas in high-income countries, the majority of transfusions (up to 76%) are given to individuals over the age of 60.
- Based on a sample of 1000 individuals, the rate of blood donations per population is 31.5 donations in high-income countries, 16.4 donations in upper-middle-income countries, 6.6 donations in lower-middle-income countries, and 5.0 donations in low-income countries.
- Between 2008 and 2018, there has been an increase of 10.7 million blood donations from voluntary unpaid donors. Currently, 79 countries collect more than 90% of their blood supply from voluntary unpaid donors, but in 54 countries, more than 50% of the blood supply comes from family/replacement or paid donors.
- Out of the 171 reporting countries, only 56 produce plasma-derived medicinal products (PDMP) through the fractionation of plasma collected within their own borders. In 91 countries, all PDMPs are imported, while 16 countries reported no use of PDMPs during the reporting period, and 8 countries did not provide a response.
- The volume of plasma available for fractionation per 1000 population varies significantly among the 45 reporting countries, ranging from 0.1 to 52.6 liters, with a median of 5.2 liters.
National blood policy and organization
The provision of safe and sufficient blood transfusion is crucial for saving lives and improving healthcare outcomes. However, many patients in need of transfusions face challenges in accessing timely and safe blood supplies. Therefore, it is vital for every country to incorporate the provision of safe blood as an essential component of their national healthcare policies and infrastructure.
To ensure effective coordination and integration of blood-related activities, the World Health Organization (WHO) recommends that countries establish national blood systems. These systems should encompass all aspects of blood collection, testing, processing, storage, and distribution. A national blood policy and legislative framework should govern the operations of the system, aiming to promote standardized implementation of quality and safety standards for blood and blood products.
According to data from 2018, 73% of reporting countries, which amounts to 125 out of 171, had already developed a national blood policy. Additionally, 66% of reporting countries, or 113 out of 171, had specific legislation in place to ensure the safety and quality of blood transfusion. This legislation covered:
- 79% of high-income countries
- 63% of middle-income countries
- 39% of low-income countries.
These figures highlight the progress made in establishing policies and legislation to support safe blood transfusion practices, although further efforts are needed, particularly in low-income countries, to enhance the availability and accessibility of safe blood supplies worldwide.
Blood Supply
Globally, approximately 118.54 million blood donations are collected each year. Out of these, 40% are obtained in high-income countries, even though these countries only account for 16% of the world’s population.
Around 13,300 blood centers across 169 countries report collecting a total of 106 million blood donations. The number of donations received by blood centers varies based on the income group of the countries. In low-income countries, the median annual donations per blood center is 1,300, while in lower-middle-income countries, it is 4,400, and in upper-middle-income countries, it is 9,300. In comparison, high-income countries have a median of 25,700 annual donations per blood center.
There is a significant disparity in access to blood between low-income and high-income countries. The whole blood donation rate is an important indicator of the availability of blood in a country. In high-income countries, the median blood donation rate is 31.5 donations per 1000 people. This figure is 16.4 donations per 1000 people in upper-middle-income countries, 6.6 donations per 1000 people in lower-middle-income countries, and 5.0 donations per 1000 people in low-income countries.
Among the countries surveyed, 60 of them reported collecting fewer than 10 donations per 1000 people. These countries include 34 in the WHO African Region, four in the WHO Region of the Americas, four in the WHO Eastern Mediterranean Region, four in the WHO European Region, five in the WHO South-Eastern Asia Region, and nine in the WHO Western Pacific Region. All these countries fall into the low- or middle-income category.
Blood Donor
When it comes to the gender profile of blood donors worldwide, approximately 33% of blood donations are made by women, although this percentage varies greatly. In 15 out of the 113 reporting countries, less than 10% of donations come from female donors.
Examining the age profile of blood donors reveals that, proportionally, a larger number of young people donate blood in low- and middle-income countries compared to high-income countries. Understanding the demographic information of blood donors is crucial for developing and monitoring recruitment strategies.
There are three types of blood donors: voluntary unpaid donors, family/replacement donors, and paid donors. To ensure an adequate and reliable supply of safe blood, it is essential to have a stable base of regular voluntary unpaid donors. This group of donors is also the safest, as they have the lowest prevalence of bloodborne infections. The World Health Assembly encourages all Member States to establish national blood systems based on voluntary unpaid donations and strive for self-sufficiency.
According to data reported to the World Health Organization (WHO), there has been a significant increase in voluntary unpaid blood donations in low- and middle-income countries. Between 2008 and 2018, 119 countries reported an increase of 10.7 million donations from voluntary unpaid donors. The South-East Asia Region witnessed the highest increase (127%), followed by the Region of the Americas (81%) and Africa (81%). In absolute numbers, the Western Pacific Region reported the greatest increase (4.15 million donations), followed by South-East Asia (3.05 million) and Africa (1.53 million donations).
79 countries collect over 90% of their blood supply from voluntary unpaid donors, including 38 high-income countries, 33 middle-income countries, and eight low-income countries. Among these countries, 64 rely on voluntary unpaid donors for 100% or more than 99% of their blood supply.
On the other hand, in 54 countries, more than 50% of the blood supply still depends on family/replacement and paid donors. This includes eight high-income countries, 36 middle-income countries, and 10 low-income countries.
‘eBloodServices’ Mobile App
In June 2020, the launch of the ‘eBloodServices’ Mobile App by Dr. Harsh Vardhan marked a significant milestone for India. Developed by the E-Raktkosh team of the Centre for Development of Advanced Computing (CDAC), this application is a notable initiative under the Digital India scheme introduced by Prime Minister Shri Narendra Modi in 2015. The app focuses on facilitating access to blood services, demonstrating the scheme’s commitment to leveraging technology for the benefit of the people. With the eBloodServices App, individuals can request up to four units of blood at a time, and the blood bank will reserve it for a maximum of 12 hours, providing a convenient solution for those in need. This innovative platform effectively streamlines the process of accessing blood units at the Indian Red Cross Society’s National Headquarters (IRCS NHQ).
| What is e-Raktkosh? |
| On April 7, 2016, the honorable Minister of Health and Family Welfare, Sh. J P Nadda, inaugurated eRaktKosh. This platform is designed to enforce the Drug & Cosmetic Act, as well as national blood policy standards and guidelines.
It aims to ensure the proper collection and donation of blood, as well as effective management and monitoring of its quality and quantity. To facilitate its nationwide implementation, e-Rakt Kosh has been developed with a modular and scalable approach, featuring a configurable rule-based architecture that allows customization to accommodate specific requirements from stakeholders across the country. |
National Blood Policy 2002
In April 2002, the government implemented the National Blood Policy (NBP) with the aim of establishing a robust system for ensuring a sufficient and safe blood supply in India. As part of this policy, the Drugs Controller General of India (DCGI) was established at the central level, along with Drug Controllers in the states. Their primary responsibilities include maintaining the quality standards of blood banks and monitoring their operations.
The introduction of the DCGI and state-level Drug Controllers plays a crucial role in regulating and supervising the functioning of blood banks across the country. These regulatory bodies are responsible for enforcing quality control measures, ensuring adherence to safety protocols, and conducting inspections and audits of blood banks. By implementing these measures, the government aims to enhance the overall quality and safety of blood transfusions, thus safeguarding the health and well-being of individuals receiving blood and blood products.
The establishment of the NBP and the regulatory bodies reflects the government’s commitment to maintaining high standards in the field of blood banking. These efforts are essential for building public trust, promoting accountability, and ensuring the availability of safe and reliable blood for medical purposes.
Objectives of National Blood Policy 2002
- To reiterate firmly the Govt. commitment to provide safe and adequate quantity of blood, blood components and blood products.
- To make available adequate resources to develop and reorganize the blood transfusion services in the entire country.
- To make latest technology available for operating the blood transfusion services and ensure its functioning in an updated manner.
- To launch extensive awareness programmes for donor information, education, motivation, recruitment and retention in order to ensure adequate availability of safe blood.
- To encourage appropriate clinical use of blood and blood products.
- To strengthen the manpower through human resource development.
- To encourage Research & Development in the field of Transfusion Medicine and related technology.
- To take adequate regulatory and legislative steps for monitoring and evaluation of blood transfusion services and to take steps to eliminate profiteering in blood banks.
(Source: https://naco.gov.in/sites/default/files/National%20Blood%20Policy_0.pdf)
India Hypertension Control Initiative (IHCI)
The Indian Hypertension Control Initiative (IHCI) is a collaborative effort involving the Ministry of Health & Family Welfare, Indian Council of Medical Research, State Governments, and WHO-India. It is a 5-year initiative aimed at addressing the pressing issue of hypertension in India. Currently, there are approximately 200 million adults with hypertension, but only around 20 million have their condition under control. To combat this problem, the Government of India has set the ambitious “25 by 25” goal, which seeks to reduce premature mortality caused by non-communicable diseases (NCDs) by 25% by the year 2025. One of the key targets within this goal is to reduce the prevalence of high blood pressure by 25% by 2025.
The IHCI plays a vital role in accelerating progress towards the NCD target set by the government. By implementing evidence-based strategies, the initiative aims to strengthen the foundational elements of hypertension management and control.
IHCI was launched in November 2017 and initially covered 26 districts across five states: Punjab, Kerala, Madhya Pradesh, Telangana, and Maharashtra. Over time, the initiative expanded its reach to include 52 districts across ten states: Andhra Pradesh, Chhattisgarh, Karnataka, Kerala, Madhya Pradesh, Maharashtra, Punjab, Tamil Nadu, Telangana, and West Bengal. This expansion demonstrates the commitment to scaling up efforts and making a broader impact on hypertension control and management in India.
The Government of India has introduced a population-based screening program for hypertension, diabetes, and breast, cervix, and oral cavity cancers. In conjunction with this program, the IHCI initiative has been launched to complement the screening efforts and accelerate progress towards the Government of India’s targets by ensuring a seamless continuum of care. The IHCI project focuses on several key activities:
- Adoption of standardized treatment protocols: IHCI works closely with State-level stakeholders to establish and implement standardized treatment protocols for hypertension management. These protocols are in line with national and global policies, promoting consistent and effective care.
- Availability of recommended drugs: IHCI emphasizes the importance of making the recommended protocol drugs readily available in all public health facilities. This ensures that patients have access to the appropriate medications for their condition.
- Task-sharing and team-based care: The initiative promotes task-sharing and team-based care, involving Auxiliary Nurse Midwives (ANMs) in activities such as blood pressure monitoring and providing drug refills to patients who have initiated treatment. This approach optimizes healthcare delivery and improves patient outcomes.
- Monitoring health system indicators: IHCI implements monitoring systems to track blood pressure measurements and other relevant health system indicators. This enables effective monitoring and evaluation of the program’s progress and performance.
- Support for implementation science: The initiative provides support for implementation science, aiming to promote continuous quality improvement. By applying evidence-based practices and fostering a culture of learning, IHCI strives to enhance the quality and effectiveness of hypertension management and control.
The IHCI initiative relies on the expertise and support of two key roles: Cardiovascular Health Officers (CVHOs) and Senior Treatment Supervisors (STSs). CVHOs are public health professionals who are recruited at the state and district levels to actively contribute to the implementation of the project. They collaborate closely with the government to operationalize the initiative, providing valuable support through activities such as supportive supervision, monitoring and evaluation, and advocacy. The presence of CVHOs at the state and district level is instrumental in ensuring the successful rollout of the IHCI.
In addition to CVHOs, the IHCI initiative also employs Senior Treatment Supervisors (STSs) who are non-medical graduates. These individuals are deployed at the sub-district level and work in conjunction with CVHOs to assist in supervision and monitoring tasks. The STSs play a crucial role in providing support to the CVHOs, thereby enhancing the effectiveness of the initiative at the grassroots level. Their involvement helps strengthen the overall supervision and monitoring mechanisms of the IHCI project, contributing to its success in combating hypertension and improving cardiovascular health.
Five Technologies For Effective Blood Management Systems In India
Medical-Grade Cold Chain Solutions
Proper storage and transportation of blood and its components are crucial to maintain their quality and prevent wastage. It is essential to preserve their biochemical composition and chemical integrity by maintaining the appropriate temperatures. In this regard, modern medical-grade refrigeration solutions play a vital role. Specialized equipment such as Blood Bank Refrigerators, Plasma Storage Freezers, and Ultra-Low Freezers are utilized for storing blood and its components at specific low temperatures, ranging from 2°C to 6°C, -41°C to -20°C, and -86°C to -20°C, respectively. These advanced devices are integrated with state-of-the-art software that enables efficient monitoring, including the acquisition, recording, and visualization of temperature data.
Contact Shock Freezers for Plasma
Contact Shock Freezers are utilized by blood banks and transfusion centers for rapid plasma freezing. These specialized freezers are designed to freeze plasma to a core temperature of -30°C or lower in the shortest duration possible. Their primary purpose is to facilitate instant freezing, ensuring efficient preservation of the plasma. Swift freezing of blood plasma is critical in preventing the degradation or loss of Factor VIII, a vital protein responsible for blood clotting.
Solar Powered Blood Bank Refrigerators
In remote areas with unreliable power supply, solar-powered blood bank refrigerators offer sustainable and dependable solutions for storing blood. These refrigerators are directly powered by solar energy and are specifically designed to minimize the loss of cold air when the doors are opened. They feature audio-visual alarm systems, remote temperature monitoring, and robust insulation to ensure that the required temperature is maintained even in situations of limited or no sunlight. By reducing dependence on grid-connected electricity, these refrigerators efficiently support the maintenance of optimal storage temperatures.
RFID Technology
Blood banks and blood management systems utilize Radio Frequency Identification (RFID) devices for the efficient management of blood sampling data and tracking of blood bags using bar-coded tags. RFID technology employs radio waves to passively identify tagged objects, enabling the reduction of human errors and the prevention of incidents such as incorrect blood transfusions. Recently, a pilot project was introduced in two prominent hospitals in Tamil Nadu, incorporating RFID technology. There are future plans to extend this system to other hospitals across the country, enhancing blood management processes.
Automated Blood Management Systems
Blood collection and transfusion centers are adopting advanced automated blood management systems that leverage cutting-edge web technologies, data analytics, Machine Learning (ML), cloud computing, and Internet of Things (IoT) devices. These innovative solutions enable streamlined processes for blood sample screening, storage, testing, and cross-matching of donors and recipients. By automating these routine tasks, these technologies minimize the need for extensive human intervention and effort.
Notes and Development
- Science NCERT Textbook Class 9th & 10th.
- Biology NCERT Textbook Class 11th & 12th.
- Campbell Biology

 Punjab Police Constable Exam Date 2025 A...
Punjab Police Constable Exam Date 2025 A...
 Punjab Police Constable Admit Card 2025 ...
Punjab Police Constable Admit Card 2025 ...
 Mahuadanr Wolf Sanctuary: India’s Firs...
Mahuadanr Wolf Sanctuary: India’s Firs...